- Homepage
- Trainees
- Examinations
- Examinations by Specialty
- Veterinary Clinical Pathology
Veterinary Clinical Pathology
Veterinary clinical pathology includes the core areas of:
- Clinical Biochemistry and Other Testing (including biochemistry, endocrinology, ELISA tests, blood gas and acid-base evaluation, and protein electrophoresis)
- Haematology/Coagulation
- Urinalysis
- Miscellaneous Topics (including the light microscope, miscellaneous equipment, Pharmaceutical/Toxicological Pathology and other types of testing)
- Cytology/Histology
- Laboratory Quality and Management
Part 1
Veterinary Clinical Pathology Part 1 Examination
Format and structure of the Part 1 Examination
Candidates will usually sit the Part 1 examination after two years’ training when the candidate is in a full-time training post. Where candidates combine training with other duties, a longer training period is likely to be required.
The written component consists of two 3-hour papers comprising of 20 compulsory short answer questions. There will be an emphasis on understanding of general pathology, pathophysiology, theory and methods for haematology, biochemistry and other types of testing, cytology and laboratory quality management.
The SAQs are designed to test factual knowledge and understanding across the range of the Curriculum. Each question comprises a stem and six sub-questions. The stem defines the topic of the question and may include a short scenario or vignette. Each subquestion is designed to elicit a specific piece of information, or demonstration of understanding of the topic and its context. Unless stated otherwise, the answer required will relate specifically to the material provided in the stem and not to the topic in general.
Points to note:
- SAQs are criterion-marked against an explicit model answer
- Marks are only awarded for information required by the question – no marks are available for additional material
- If a defined number of facts are requested (e.g. State two causes of…..), only that number of responses will be marked (e.g. Answer – correct cause, incorrect cause, correct cause, will only receive one out of two marks).
- Answers requiring more than single word or phrase responses will be answerable in a single sentence or a small number of sentences.
- Examiners will be looking for key concepts in these answers and no marks will awarded for extra information.
Candidates should practice writing short, concise answers, which include only the information requested. Good use of English, avoidance of abbreviations, and clear handwriting are, however, essential. Candidates who write unnecessarily long answers are likely to penalise themselves because these answers waste time.
The mark allocation for each sub-question will be stated in brackets in each instance.
Part 2
Veterinary Clinical Pathology Part 2 Examination
Part 2 Examination: Introduction
The Part 2 examination will usually be taken at least one year after successfully completing the Part 1 Examination and a further year of full time supervised diagnostic practice. Candidates will be required to provide a written recommendation from their supervisor/sponsor of fitness to sit the exam with details of activities undertaken in veterinary pathology since passing Part 1.
This guidance is produced for trainees taking the Part 2 examination. It is meant to provide general information about the approach to taking the examination and the guidelines and approach taken by examiners in marking this examination. Specific items are not covered and practice in each area with feedback from your supervisor will be crucial in developing good habits and knowledge needed to pass the Royal College of Pathologists examination in Veterinary Clinical Pathology.
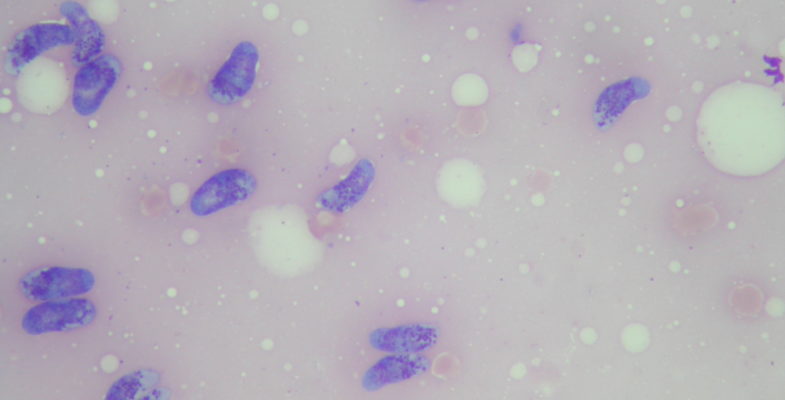
Cytology Glass Slides
GENERAL APPROACH
Most of the marks will come from the description, but it is unlikely that you will receive a passing mark if interpretations are consistently wrong or do not reflect the ability to commit to an interpretation or consistently suggest a lack of confidence in the interpretation.
The purpose of the description is to provide the examiner with the ability to ‘visualize’ what was seen in the cytologic preparation.
The purpose of the interpretation is to provide a concise, easily-read diagnosis or summary of findings. It may be a pathologic-anatomic, aetiologic and/or descriptive interpretation. A single interpretation or multiple interpretive items may be appropriate, depending on the findings in the slides.
The purpose of the comment is to communicate the degree of confidence or uncertainty of the interpretation and any differential diagnoses, recommendations for further testing or monitoring and any ‘useful information’ about the condition that you think is present.
Many descriptions can be covered adequately with 3-7 sentences, depending on the complexity of the case and the cytologic features.
Many comments can be adequately addressed in 3-5 sentences.
SPECIFIC ITEMS:
- Complete sentences are not required, but often make the reading easier and the presentation more pleasing.
- Use a methodical approach in the description and cover the same things, in the same order for each report. The following does not imply the order of description but covers those things that should be described:
- Describe the degree of cellularity and quality of the preparation and indicate any insufficiency of collection and processing of the sample for cytological evaluation
- Describe the background (clear, proteinaceous, mucinous, etc)
- Describe the cells that are present. Use semi-quantitative modifiers such as few, moderate or many/marked. This is better than saying ‘some’ or ‘several’.
- Quantitative descriptors for size of cells and absolute or relative numbers should be included, when appropriate. These may be comparisons of various cells or features relative to erythrocytes or leukocytes or per field of view (medium-sized lymphoid cells whose nuclei are 1.5-2.5x the diameter of erythrocytes, 3-5 mitotic figures per high power field [100xoil]).
- Describe any cellular relationships that are present (discrete cells, loosely associated groups, cohesive groups, papillary or acinar configurations, etc).
- If description of the cells is needed (not just identification of the cell type), then either start with the nucleus and then move out to the cytoplasm or vice versa.
- When describing nuclei, be sure to include size, shape, location, staining, chromatin pattern and if there are any inclusions. Also the nuclear to cytoplasmic area ratio should be indicated and how variable it is.
- When describing nucleoli, be sure to include size, shape and location (central vs peripheral), prominence and number / nucleus. The variation in these parameters should also be indicated.
- When describing the cytoplasm, include shape(or range of shapes represented), colour, staining intensity and distinctiveness of the cell boundaries, contents (such as granules, vacuolation, etc.).
- Mitotic figures should be mentioned with an estimate of frequency (none, rare, frequent) and whether atypical mitotic figures are present (tripolar, trailing chromosomes etc).Describe any infectious agents. With yeast it is important to include size, shape and presence of any capsule or ‘halo’ associated with the organism. If budding is present, describe it (frequent, few, narrow-based, broad-based, etc).
- If fungal hyphae are present, describe the width, whether or not septae are present and the type of branching (dichotomous, right angles, frequent, infrequent, etc.). For bacteria, include whether these appear to be rods, cocci and /or coccobacilli and the distribution (single, in chains, in clusters) and location (intracellular, extracellular, cell-surface-associated). For protozoa, describe size, any internal structure or identifying features (kinetoplast, capsule, etc.)
- Describe any other features or noncellular material that may be present (crystals, extracelluar matrix material, pigment granules, etc) .
3. With some cytological findings, it may be of benefit to specify when certain things are not seen, such as infectious agents with suppurative inflammation, or cells with features of malignancy with benign neoplasia, or in vivo indicators of haemorrhage with apparent iatrogenic haemorrhage. This will indicate that you looked specifically for these features and diagnoses and that they are not present and can be excluded.
4. For the interpretation, give the diagnosis as far as , but only to, the extent that can be supported by the cytological findings. Qualitatively indicate the degree of uncertainty for this diagnosis:
Example: You may be comfortable saying it is ‘Epithelial neoplasia’ or ‘round cell neoplasm’ vs. Adenocarcinoma or amelanotic melanoma or may include modifiers such as ‘probable’, ‘likely’, ‘suggestive of’ or ‘consistent with’.)
The interpretation is the reason that the clinician has submitted the sample and should provide a clear and full understanding of the diagnostic significance of the cytological findings to the reader.
Then use the comment to explain your degree of confidence and additional information (see item 4). There may be multiple items included in the interpretation, for example:
- Haemorrhage and/or contamination with blood, marked
- Inflammation, purulent to pyogranulomatous, moderate to marked
- Bacteria, rods, extracellular and intracellular, many).
Your presentation of these should be in a way that is easy to read and understand.
In the comment indicate the non-cytological information that supports your cytological interpretation, such as if there is a strong association with breed, anatomical location, lesion description, the clinical signs. history, or if there is a high incidence of a particular diagnosis with some of the presenting cytological features.
5. In the comment, do not rehash why you made the decision you have made in t he interpretation. The purpose of the comment is to provide useful information to the clinician and to communicate the degree of confidence you have in the interpretation that you have made.
- Communicate the degree of confidence you have in the interpretation (Ex: Mesenchymal neoplasia is considered most likely, but a focus of active fibroplasia cannot be ruled out; The low degree of cellularity is not typical of most mast cell tumours, so an inflammatory reaction that includes mast cells also should be considered).
- Give some information about the expected biologic behavior of the condition, if appropriate (Ex: metastases are uncommon; regional lymph node metastases are common at the time of diagnosis; oral malignant melanoma is an aggressive tumour and evaluation for regional and distant metastases is recommended, etc).
- Include differential diagnoses, if appropriate.
- Specifically indicate any insufficiency in the quality and quantity of the cytological specimen and what limitations this may have had on cytological assessment, and if there is a subsequent need for corrective action and re-submission.
- Specifically indicate if there is a need for biopsy for histological evaluation or confirmation. Also, include information about any additional testing or monitoring that may be done, if appropriate.
- Be sure to address any correlation with the clinical signs (this is expanded on and separated out in part 4 above)or address any questions included in the history.
Haematology Glass Slides
GENERAL APPROACH AND PHILOSOPHY
The purpose of the haematology write up is to confirm the automated findings and relate the findings to the clinical signs or questions presented in the history, as well as to provide an interpretation of the findings and useful information about the significance of the findings or conditions that are present.
The general principles of the cytology report apply, but description is usually more limited than for a non-haematological cytology specimen. Detailed descriptions of cells, infectious agents or other features are usually limited to those things which are not routinely present in blood and which need a description in order for the reader to visualize what was seen in the preparation.
SPECIFIC ITEMS:
- Description for a haematologic specimen is usually shorter than that associated with a cytological description, but should include a brief description of the Erythron, Leukon, Thrombon and any other features (Ex: infectious agents, foreign material, unusual cell types or features, presence of artifacts, etc.):
- Unless anaemia is severe, it is extremely difficult to make any evaluation of the density of erythrocytes relative to the presence of anaemia, so this evaluation is usually addressed only in extreme cases. Characterization of the erythron should be included. Note : cell counts are provided where needed. Red cell morphology should be described.
- The density of leukocytes is pertinent and should be related to the automated WBC (Ex: there is a marked increase in the density of leukocytes that confirms the markedly elevated automated WBC count, etc.) An estimated percentage of WBC types should be stated. Any unusual features or reflections of pathological conditions should be included. (Ex: toxic changes, hyposegmentation of nuclei, atypical vacuolation, blast cells, etc.)
- The platelet estimate and platelet morphology is important. Any clumps that may result in artefactual thrombocytopaenia based on the automated platelet count should be mentioned.
- Any other features, including infectious agents, extracellular material or other findings should be included.
- The interpretation should be as specific as possible based on your confidence in formulating it
- The comment should include some information:
- about the confidence in your interpretation (Ex: the combination of strongly responding, macrocytic-hypochromic anaemia with moderate leukocytosis with neutrophilia with a left shift and the presence of moderate numbers of spherocytes provides strong support for immune-mediated haemolytic anaemia).
- Useful information about the condition (s) identified
- The relationship of the morphologic findings and automated findings and clinical signs
- Recommendations for any additional testing or monitoring that may be of benefit (and why).
- Bone marrow smears may be included in the haematology section along with a partial CBC report. Description should include comments on the overall cellularity and amount of blood contamination, if present. Mention should be made of erythroid and myeloid series cells and an estimate of an M:E ratio made. Monocytic series cells and megakaryocytes should be mentioned. The presence of iron reserves, plasma cells, lymphocytes or other cell types should be noted. Maturation of cells, and synchrony between nuclear and cytoplasmic differentiation should be commented on if appropriate.
Candidates should practice looking at bone marrow smears and estimating cell populations without doing a 300-500 cell count. Doing 300-500 cell counts is useful during the learning stages of bone marrow evaluation, but is not expected or suitable for the purposes of this examination. Interpretation with the same qualifiers as used in the cytology. descriptions is essential
- A suggested diagnosis should be made. (Example: marked hyperplasia with erythroid hyperplasia in response to the anaemia Infiltration of atypical neoplastic cells Myeloid hypoplaisa marked ). If appropriate a comment on differentials and further testing can be provided
Clinical Case Write Ups
GENERAL APPROACH AND PHILOSOPHY:
The purpose of the clinical case writeup is to determine if the candidate is able to :
- recognize patterns of clinico-pathological findings that suggest or support specific or general clinical conditions or diagnoses
- understand the basic pathophysiology and mechanisms underlying the clinico-pathologic findings
- relate the clinico-pathologic findings to the reported clinical signs and questions included in the history
- identify circumstances where findings can or cannot be explained by a single condition, diagnosis or clinical syndrome and communicate clearly any changes which are not typical of the suspected clinical condition, diagnosis or clinical syndrome.
- provide differential diagnoses for combinations of findings, when appropriate (note: every differential for every single abnormality need not be covered)
- provide information about additional testing or monitoring that may be needed based on the presented findings
- communicate concisely and coherently in writing. The write-up should be easy to read, and demonstrate logical reasoning and precise presentation. of this information.
Most clinical case write-ups should be dealt with in several pages using a series of paragraphs, Occasional complicated cases,or cases with groups of animals may require more pages.
SPECIFIC ITEMS:
- Group analytes and address combinations or patterns of abnormalities according to organ system. Some analytes will need to be included in several organ systems (Ex: AST will be included in analysis of liver and muscle; Albumin may be related to liver, urinary system, and GI tract).
- You may include analytes or aspects from several types of analyses to provide support for a particular condition or clinical syndrome (Ex: may include certain things from haematology, biochemistry and urinalysis together)
- Make a commitment to what you think the underlying condition(s) or clinical syndrome(s) are (if possible) , with appropriate differential diagnoses (if any).
- Indicate what findings are not explainable or typical of the suspected clinical condition(s) or syndrome(s) that you think are present.
- You may include additional testing recommendations within the writeup or as a separate section at the end of it. It may be easier to include these as you write the case since it is easier to determine what findings the additional testing is being suggested for and why, while you are doing the analysis of the information. provided
- Read through the case and consider the combinations of findings initially, BEFORE starting the write-up.
- Check off abnormal data as you deal with it in the write-up. That way you know when you look back that you have covered all of the abnormalities that are present in the case.
- Practice timed clinical case write-ups frequently, with review by an experienced clinical pathologist for plausibility, as well as accuracy of information and quality of presentation of the ‘thought process’. ‘Telling the story’ is an integral part of presenting the information.
Practical Examination: Summary
The practical portion of the Examination is designed to test the ability of candidates to handle the interpretation of cytology, haematology (including bone marrow specimens) and the results of a variety of laboratory tests. These tasks are those that make up a large proportion of the ‘job’ of a veterinary clinical pathologist on a daily basis. The examination process should be approached in the same practical way as you would approach these types of cases in your daily work. Practice will be needed to direct your attention to time limits for the cases, their analysis and presentation.
This is true for the cytology, haematology and cases analysis sections as well as the timed photomicrographs, which can be from any area of clinical pathology e.g. cytology, haematology with parasites bacteria extraneous materials,QC/QA material and biochemistry. These require a single sentence or a few words answers and are displayed for 1 minute each.