- Homepage
- Trainees
- Examinations
- Examinations by Specialty
- Histopathology
Histopathology
Part 1
Histopathology Part 1
Histopathology MCQ/EMQ Examination
Part 2
Histopathology Part 2 Examination
Histopathology Practical Examination
The practical examination is comprised of 6 components taken over 2 days:
Surgical histology
Twenty cases will be provided in 10 pairs of haematoxylin and eosin (H&E) stained slides in 20-minute slots over
3 hours 20 minutes on the second morning, and is a written component of the exam. The cases are blueprinted to the curriculum and include a balanced mixture of neoplastic and non-neoplastic material. The cases are drawn from a wide range of organ systems including upper and lower gastrointestinal tract, gynaecological tract, breast, skin, soft tissue, osteoarticular, respiratory, urological, lymphoreticular and endocrine systems. This list is not comprehensive. The cases will represent a range of difficulty from straightforward cases readily diagnosable on a single H&E section, more complex cases requiring more detailed description, differential diagnosis and special techniques, and cases not capable of diagnosis on a single H&E which should prompt an approach for further techniques, extra blocks and specialist opinions. The overall level is designed to recognise pathologists close to the end of training, such that they demonstrate an appropriate approach to independent practice. The responses will be marked centrally according to pre-determined criteria, using the closed marking system.
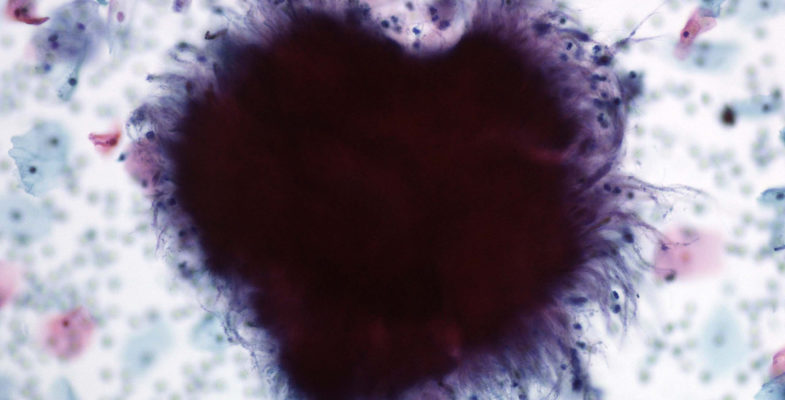
Cytopathology
Eight non-gynaecological cytology cases will be provided in pairs in 20-minute slots on the first morning of the examination. The responses will be marked centrally according to pre-determined criteria, using the closed marking system. This is a written component of the examination.
Long Cases
These are 4 x 20-minute stations. They will include cases which cannot conventionally be covered by a single H&E stained section and require additional stains such as immunohistochemistry (tumours and lymph nodes), immunofluorescence (skin and renal biopsies) and electron microscopy (renal biopsies) This list is not exhaustive and other types of cases may also be used.
The responses will be marked centrally according to pre-determined criteria, using the closed marking system.
This is a written component of the examination.
Macroscopic Pathology
Four cases will be provided in the form of photographs of gross pathology specimens. Candidates will be provided with clinical information and will be asked to prepare their responses to specific questions and to mark on the photographs where they would take blocks. Two 20-minute slots will be provided to view 2 cases per slot, followed by a 20-minute discussion with 2 examiners. This section is marked on the basis of discussion with the examiners only and not a candidate's written preparatory notes. This section is designed to allow candidates to demonstrate their capabilities in discussing gross pathology and familiarity with block selection in the context of the RCPath Minimum Datasets. Each case is marked to a pre-determined marking scheme.
OSPEs
These are 2 x 20 minute stations: OSPE1 is conducted face-to-face with 2 examiners while OSPE2 is a written exercise only. Possible topics include management/clinical governance type and MDT type cases, although this list is not exhaustive.
Frozen Sections
There will be 6 cases to be viewed in 2 x 20-minute stations (3 cases per station) before meeting with a pair of examiners in a 20-minute station. Candidates should make notes, to form the basis for face-to-face discussion with 2 examiners who will expect a discussion consistent with the report given to the requesting surgeon. This section is marked on the basis of discussion with the examiners only and not a candidate's written preparatory notes.
Each case is marked to a pre-determined marking scheme.
Certificate of Higher Autopsy Training
CHAT Examination
Phase 1 - Practical Assessment
In order to proceed to the Phase 2 OSPE, candidates have to satisfy examiners that they can dissect a cadaver, examine the organs, and provide a cause of death and/or a plan of further investigatory action.
This involves the performing of a routine autopsy examination. This could include a standard post-operative death but not multiple complex surgeries, high risk cases, decomposed body or poly-trauma. Within a diet, candidates can have 2 attempts at this phase, which should take place in the candidate’s own mortuary or another where he/she wishes to be examined. The examiners should be one local consultant (perhaps the educational supervisor), and another from an adjacent region. The outcome will be pass or fail: i.e. satisfactory and proceed to phase 2 or unsatisfactory
The candidates should demonstrate a risk assessment with safe practice, within standard health and safety protocols, with professional interactions with the examiners.
The candidates are encouraged to call for the examiners to debate various aspects during the course of the exam, rather than waiting for the final discussions.
The candidate should show understanding of the case background, careful tissue dissection, analysis and a basic discussion of the findings to the two examiners.
The candidate will be expected to have knowledge of normal dissection techniques, the appearance of tissues in normality, expected organ weights and to be able to identify relevant pathologies. Discussions about tissue sampling and organ retention may be seen as reasonable and basic devices (pacemakers, valves and coronary stents) will often be encountered.
The dissection should be completed with 90–120 minutes, although additional time will normally be allowed for complex cases. The examiners decide whether or not the candidate has passed this phase and inform him/her at the time. If it is a fail, they provide constructive feedback.
Phase 2 - Centralised OSPE
The OSPE examination will take place at 1 location, it will comprise 14 questions overall of 15 minutes' duration, with 2 of these being viva stations.
The OSPE tests knowledge, skills and attitudes in various scenarios and includes questions on aspects of autopsy work. A working knowledge of the Coroner’s system of England,Wales and Northern Ireland and the Crown Office and Procurator Fiscal Service of Scotland, and the Human Tissue Authority rules.
Toxicology/biochemical pathologies:
Metabolic deaths, including diabetes.
Toxicological samples required in specific circumstances.
Drug toxicities that occur within toxicology reports: paracetamol, aspirin, opiates (codeine, morphine, heroin, methadone, fentanyl, nitazenes and novel opioids) pregabalin, gabapentin, benzodiazepines.
Commonly misused stimulants (cocaine, amphetamine, spice/novel psychoactive substances). A basic working knowledge of barbiturates, nitrous oxide, antidepressants, common cardiovascular drugs, anti-epileptics and lithium.
Reference ranges of drugs are given.
Post-operative pathology
These cases feature regularly at autopsy practice and candidates should be aware of complications possible during and following common surgical procedures. Examples might include colonic resections, gastrectomy, lung lobectomy, aortic/cardiovascular surgery. The candidate will be expected to have a basic understanding of standard post-operative pathologies and how they may cause deaths plus how other therapies might contribute to death.
No unusual or rare surgical procedure case would feature in this part of the exam, unless it was deemed to have been explained sufficiently so that general case understanding was possible.
The candidate may be asked to explain the consequences of the pathologies, the relevance of various diagnostic tests and the choices of histological sampling. The role of microbiology and biochemistry tests may be part of the question.
Post-mortem CT scan cases (PMCT)
All CHAT exams currently have at least one question dealing with this post-mortem study technique, which reflects the rise of PMCT across the UK and beyond. It is assumed that the candidates will have had exposure to various radiological imaging techniques as part of their medical training and early years professional work.
The CHAT exam notes that not all centres have exposure to PMCT. All candidates progressing to the CHAT exam will need to have read some basic text data around the subject and ideally to have attended some teaching on this technique. Even candidates with low exposure to PMCT should not be disadvantaged, as the basic reality is that PMCT is analogous to an open autopsy requiring analytical consideration of the data presented.
The candidates are expected to read a case scenario, to consider the data of the external features reported and then to review the PMCT radiological report. No images of the radiology are presented. The questions likely to be posed will prompt the candidate to answer whether the radiological (PMCT) is sufficient to define a cause of death, or whether an open autopsy is required (full or limited). Or whether additional investigations are required.
Appreciation of the wishes of the relatives may be part of the understanding of the case.
Sudden death cases, often reflecting the College scenarios
These principally revolve around the various autopsy scenarios published on the College of Pathologists’ website relating to adult and maternal deaths.
The questions allow candidates to demonstrate knowledge of the scenario concepts and to apply the knowledge within the question posed. This might involve analysing case data, macroscopic and microscopic findings and aspects of Health and Safety. The investigations of relevance to these cases, alongside any specific dissection techniques.
The need to refer some samples (hearts, brains, etc) for other tests should be understood, but not overplayed.
Health and safety Scenarios
These questions usually consider aspects of post-mortem work in order to test appreciation of autopsy room hazards and safe practice. This includes knowledge of appropriate
personal protective equipment (PPE) for different categories of pathogen, high risk protocols and risk assessments of doing a post mortem.
The roles of vaccination and risk assessment for health staff and appreciation of contact tracing should be part of the knowledge for the candidates. The relevance of correct samples being taken for analysis is occasionally assessed and may feature as part of the question.
Unusual circumstances for autopsy cases may be presented for consideration. These might include those bodies that have been exposed to highly toxic chemicals or radionuclides.
Macroscopic and histological images
The autopsy images are usually presented on a tablet-type computer.
Macroscopic images can be from any of the range of pathology or normal findings encountered at post-mortem. This can include natural and unnatural deaths.
Histological questions might include pathologies that are relevant to the cause of death or common post-mortem artefact. They may relate to natural or unnatural death.
Candidates are recommended to review as much histology from their centres in the preparation period before the exam.
Complex medical cases
The scenarios of complex autopsy data generally revolve around disease/s in multiple different organ systems, being principally cardiovascular, respiratory, central nervous system and kidney. These scenarios may involve pathologies, complicated by previous procedures and/or treatments.
The candidate is expected to consider the poly-pathology cases and then to consider which pathologies are most important and relevant to the cause of death, and which are distractions (ie. not relevant to the cause of death).
One of the common components of this question is the need to produce a cause of death in the standard ONS format.
Alternatively, the candidate may be required to produce an analysis of the components of disease that have led to death. The candidate might be asked to identify a failure to provide a surgical interaction or medical therapy that could have changed the patient’s outcome.
Industrial disease
Occupational disease remains a common feature in the autopsy exam, with a strong focus on lung disease. Asbestos, silica and coal dust often present as text and/or image-based questions.
Asbestos-related pathology remains commonplace in terms of autopsy practice. Candidates are expected to know about the main pathologies caused by asbestos (persistent pleural effusion, diffuse pleural fibrosis, diffuse interstitial lung fibrosis, lung carcinoma and mesothelioma) as well as the issue of pleural plaques. Awareness of the College guidelines/scenarios on this type of case is often tested, along with basics of fibre identification and the Helsinki criteria.
Silica and coal dust -related pathologies are less common in terms of autopsy practice than previously, but there are some questions possible at the autopsy exam. These might involve the interpretation of images or an understanding of the common pathologies that reflect these two dusts. For coal dust, the link with chronic obstructive pulmonary disease, dust macules, dust nodules, progressive massive fibrosis and Caplan’s syndrome are expected knowledge. For silica, the macules and nodules are also expected to be understood along with the issue of diffuse lung fibrosis. The potential link/or not to lung cancers is expected to be known for these two dusts.
Industrial disease can also be an aspect of unnatural death and trauma. An understanding of the mechanisms of death in major trauma is expected, and what further testing might be necessary.
Interactive (face:face) stations
There are two stations, both of which involve direct questions from two examiners. The stations have a dedicated preparation time for review of case data such as written or image material prior to entering the face to face room.
The examiners will normally ask questions to check that the candidate understands the key points of the pathology and is able to correlate data accordingly. Often, the candidate is asked to formulate a cause of death and to present the information in a way that would be useful to a family or the Coroner, as if in court.
The candidate may be asked to consider or refute a challenge from an examiner acting as the coroner or a relative, again, as if in courtroom.
The questions may revolve around exclusion of alternate diagnoses and the implications of a diagnosis for the family. The candidate will be expected to discuss the data in a manner suitable for court or direct interaction with the relatives (interchangeably using both medical and layman’s terminology).
Alternatively a scenario could involve interpretation of a post mortem report, a CT-PM report or consent for a hospital post mortem or organ retention with possible genetic testing.
Points are also given for the correct answers given and the communication skills demonstrated.
Certificate of Higher Cervical Cytology Training
CHCCT Examination
CHCCT Examination
The cervical cytopathology examination is intended for candidates who wish to carry on and pursue higher training in Cervical Cytopathology. Successful completion of this component will result in the award of the Certificate in Higher Cervical Cytopathology Training (CHCCT).
The examination will consist of 2 sessions over 1 day.
The morning session: Twenty single slide cases over a period of 3 hours and 20 minutes on the morning of the examination. For each case a short history including the age of the patient, the stage of the menstrual cycle if known and any previous abnormal cervical cytology will be provided. Additional information may be provided if appropriate. Cases will be a mix of negative and abnormal slides. Candidates will be expected to provide a brief description of the findings on the slide and to make an appropriate management recommendation based on the clinical history and the findings on the slide. It is expected that candidates will use the terminology of the NHS Cervical Screening Programme and management suggested should be in line with current guidelines that do allow for some local variations in practice.
The afternoon session: The second paper for this examination will consist of a 2 hour written paper. The questions may include an understanding of the management of a cervical cytology laboratory participating in the National Health Service Cervical Screening Programme (NHSCSP), changes and developments within the NHSCSP, and interpretation of statistical data regarding individual and laboratory performance. It should be noted that candidates will be expected to use standard NHS Cervical Screening Programme terminology and management recommendations.