- Published:
- 22 April 2025
- Author:
- Asha Aggarwal, Katrina Fordwor & Lucia Chen
- Read time:
- 3 Mins
The transition to registrar can often be challenging. This change is particularly stark in haematology, in part due to the infrequent exposure to haematological emergencies on the general medical take. A survey of new registrars in our local deanery reflected this, with most new specialty trainees (62%) feeling ‘very or somewhat unprepared’ to begin haematology on-calls. Many highlighted their anxiety in managing unfamiliar but life-threatening haematology emergencies, such as thrombotic thrombocytopenic purpura (TTP) and acute promyelocytic leukaemia (APML).
Recognising this issue, we identified simulation training as a way to address this knowledge gap. Simulation provides a realistic setting in which to learn and develop confidence in managing these scenarios, while posing no risk to patients.
We developed a half-day, multiple-scenario simulation course for new haematology registrars that aims to improve both preparedness and knowledge of haematology-specific emergency management protocols.
Running since 2022, courses take place in a hospital simulation suite, using a high-fidelity mannequin with a range of physiological functions in a faux-ward setting. Specialist simulation technicians operate the mannequin and are the ‘patient voice’ throughout the scenarios.
The emergencies simulated are new TTP, APML and a bleeding haemophilia patient. The scenarios are adjusted prior to each course to accommodate the number of attendees and modified iteratively according to participant and facilitator feedback from the previous course.
Each simulated scenario runs for approximately 20 minutes, followed by a facilitated structured debrief in which trainees actively reflect and analyse the events of the scenario to maximise individualised experiential learning. Additional real-world expertise is brought to the discussion by a subspecialty consultant or specialist nurse to solidify key management principles for each scenario. Training is interprofessional, with nurses from the haematology ward/triage unit also attending for training.
So far, we have run 5 courses, with 25 registrar attendees in total. After attending the course, trainees reported improved confidence in managing emergencies. Comparison of the pre- and post-course confidence scores demonstrated an improvement in self-rated confidence in the management of all 3 course scenarios (Figure 1).
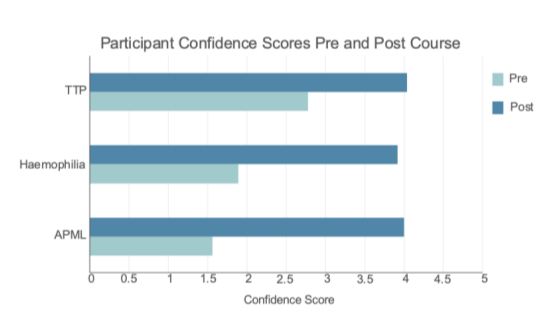
Trainees, on average, rated the course 4.42/5 for usefulness, 4.86/5 for the acquisition of new knowledge and 4.83/5 for real-life application. Trainees particularly enjoyed the interprofessional aspect of learning and felt they gained an understanding of the Trust-specific logistics of how to manage these difficult scenarios, which helped prepare them for their on-calls.
There have been challenges to delivering this course, including securing sufficient staff time and creating a sustainable pool of trained faculty to support the course. We have also had challenges obtaining long-term funding for the use of the simulation suite. Short-term solutions so far have been commercial and hospital funding. In future, we aim to expand the simulation to a whole day, facilitating the inclusion of liaison haematology and communication skills scenarios.
In summary, we have demonstrated that this novel haematology simulation programme for registrars is a feasible, efficient and effective way of upskilling new haematology registrars in managing unfamiliar specialty-specific emergencies. We believe the development of similar haematology simulation courses in other UK centres would be beneficial to the wider cohort of UK haematology trainees and we would be happy to collaborate on efforts to roll this training out elsewhere.