- Published:
- 17 October 2024
- Author:
- Anu Gunuvardhan and Meena Upadhyaya
- Read time:
- 5 Mins
A recent conference covered the significant disparities that ethnic minority women face within the Welsh healthcare system. The key themes emphasised the necessity for systemic changes in healthcare delivery and policy.
The Health Inequalities Conference was organised by Ethnic Minority Women in Welsh Healthcare (EMWWH) and held in Cardiff on 29 June. EMWWH was established in 2015 by a dedicated group of women with a deep understanding of racial and gender discrimination and its harmful effects. It is the only voluntary organisation Wales that focuses on supporting ethnic minority women in healthcare.
65% of avoidable deaths under the age of 75 could be attributed to conditions that are preventable, which underscores the existing gaps in healthcare and preventive services.1
There is an evident link between poverty and health outcomes. 28% of children in Wales live in poverty. Families in social housing who face economic deprivation and disability risk falling into a cycle of poverty across generations. It is crucial to address the social determinants of health, including housing, economic stability and education, to break this cycle and achieve health equity.
Dr Mohammad Al Hadjali and Dr Raja Biswas gave presentations that highlighted the specific health challenges faced by migrants, refugees and older people, especially those from minority ethnicities. The emphasis on health advocacy and community-based education tailored to refugees is crucial in addressing health disparities in these groups.
Similarly, the discussion on elderly care emphasised workforce challenges and the need for multidisciplinary teams to manage the complex health needs of an ageing population. The ongoing impacts of COVID-19 on older patients, especially within Bangladeshi and Pakistani communities, further illustrate the compounding effects of existing health inequalities.
Prior to COVID-19, health inequalities were estimated to cost the NHS an extra £4.8 billion a year and costed society around £31 billion in lost productivity. Between £20 and £32 billion a year was in lost tax revenue and benefit payments.2 This cost reflects financial strain and also reduced life expectancy and quality of life. The fact that the UK has one of the lowest life expectancies in Europe underscores the need for comprehensive healthcare reforms.
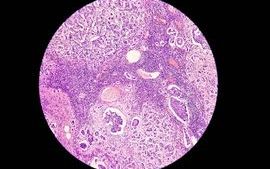
Bami Adenipekun emphasised the importance of listening to the lived experiences of patients from ethnic minority backgrounds, highlighting the need for patient-centred care. Cultural sensitivity in healthcare is essential, for example in addressing mental health and oncology outcomes among ethnic minorities.
The principle of ‘nothing about me without me’ serves as a reminder for healthcare professionals to engage with patients respectfully and inquisitively. Expertise in healthcare must be complemented by an understanding of the patients’ lived experiences.
Dr Helen Munro led a discussion on gender bias and women’s health, covering the specific health challenges faced by women that underscore ongoing inequities in healthcare. The lack of research and data collection on women’s health, coupled with bias in healthcare delivery, contributes to poorer health outcomes for women, particularly in later life.
Dr Munro emphasised that the increase in suicide rates and the heightened risk of cardiovascular disease in perimenopausal women highlights the need for targeted interventions and awareness campaigns, pointing out that gender-specific health inequalities affect both physical and mental health, as well as the quality of health expectancy beyond 65 years: furthermore, women are not generally listened to or heard by health professionals.
Dr Nadia Hickary-Bhal presented a discussion on menopause, which highlighted the unique challenges faced by women, particularly those from ethnic minority backgrounds. Studies demonstrate that ethnic minority women are more likely to experience early menopause,3 which is associated with higher morbidity and mortality rates. Barriers such as language, bias and stigma can influence the experience and management of menopause, particularly for women of colour.
Menopause is shaped by cultural perspectives. The ‘bio-psycho-cultural model’ illustrates how cultural differences affect the experience of menopause. A significant link exists between menopause and domestic abuse, especially for women aged 36–55. How menopausal symptoms are presented can affect quality of care. A holistic approach to menopause care is crucial to improve quality of life and reduce future health risks.
The acceptance of hormone replacement therapy is less common among women of colour, often due to concerns about cancer and a lack of help-seeking behaviour. There is a critical need for specialised support, a person-centred approach and access to female GPs. It is essential to be aware of symptoms and to address communication gaps. The symptoms of menopause in ethnic minority women may differ from those of White women, which leads to a lack of confidence in primary care physicians.
The conference stressed that addressing health inequalities requires a comprehensive approach, including policy reform, improved healthcare access and a focus on the social determinants of health. The Discovery report on the Foundations for a Women’s Health Plan for Wales4 and the launch of a centralised data repository are positive initiatives, but they will require ongoing effort and collaboration across various sectors.
The conference highlighted the importance of inclusive, patient-centred care and the need for healthcare professionals to engage with and understand the diverse experiences of the populations they serve. Improving healthcare and addressing health inequalities involves a multi-faceted approach that tackles the underlying causes of these differences.
The COVID-19 pandemic illuminated existing health disparities, particularly those that affect marginalised communities. Many social determinants, such as housing, education and employment, have a significant impact on health outcomes. This has necessitated interdisciplinary discussions and solutions to address these issues.
References available on our website.
Return to October 2024 Bulletin
Read next
Tackling ethnic inequalities in precision and genomic medicine
17 October 2024
Inequalities in cancer – an unequal burden
17 October 2024
Transfusion Transformation Symposium
17 October 2024