- Published:
- 17 October 2024
- Author:
- Dr Robert Danby
- Read time:
- 10 Mins
Successful transplants for blood cancer and blood disorder patients require matching donors. However, socioeconomic and genetic differences mean that some patients face disproportionately worse transplant outcomes. UK stem cell charity Anthony Nolan is leading the charge to resolve this. For this health inequalities edition of the Bulletin, Dr Robert Danby, Chief Medical and Scientific Officer at Anthony Nolan and RCPath College Fellow, expands on ongoing work to ensure all patients have an equitable opportunity to survive and thrive after a transplant.
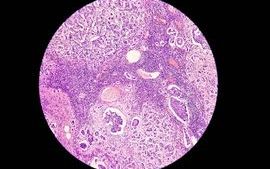
When Anthony Nolan was born in 1971 with Wiskott–Aldrich syndrome, a rare inherited immunodeficiency disorder, his mother Shirley was told a bone marrow transplant was his only chance of survival. Known today as haematopoietic cell transplant (HCT), the procedure involves replacing affected bone marrow with that of a healthy human leukocyte antigen (HLA)-matched donor. But with no siblings, Anthony would need an unrelated donor.
At the time, there was no system to find potential donors for people like Anthony. Desperate for a match for her son, Shirley set up the world’s first register of people willing to donate their bone marrow to those with blood cancers and serious blood disorders.
Sadly, Anthony died aged just 7 while waiting for a donor. But his and Shirley’s legacy remains. 50 years later, the Anthony Nolan charity currently has over 900,000 people on its register and gives 4 people a day a second chance of life by facilitating life-saving stem cell transplants.

Initially an experimental treatment, HCT is now considered a routine, though complex, therapy for thousands of patients each year with otherwise incurable blood cancers and serious blood disorders.1
As risks and complications have reduced with improved clinical understanding and new therapies, HCT has become available for a growing list of indications, including sickle cell disease and thalassaemia, and is increasingly used in older patients.2–4 In recent years, our knowledge and understanding of HCT has also become central to emerging cell and gene therapies, like CAR-T therapy (read more in the July 2024 Bulletin), where genetically engineered cells are being used to treat malignant and non-malignant conditions.5,6
But there is still work to do. The intense nature of a transplant means many patients still suffer serious short- and long-term side effects and reduced quality of life after treatment.7 On average, 5-year survival post-transplant sits at little over 50 percent.8 Furthermore, disparities in access to and recovery from transplant – due to age, ethnicity, socioeconomic status and more – mean it’s likely that many patient groups may face disproportionately worse outcomes.9
When I was appointed Chief Medical and Scientific Officer at Anthony Nolan last year, it was clear that our research strategy needed to reflect and expand on this progress, while working towards ensuring all patients could equally benefit.
Our mission to give all patients in need of a stem cell transplant the best possible outcomes has not wavered since Shirley first established the donor register. But the work we are doing to achieve this has evolved to meet the demands and opportunities in the field today.
In our new research strategy launched earlier this year, we set out 3 ambitious goals.
- Survival: transform outcomes for every patient.
- Equity: achieve greater equity of access, experience and outcomes.
- Progress: contribute to the development of new cell and gene therapies and ensure they are made available to more patients.
To achieve this, we had to rethink our approach to research. Having historically focused on the science of identifying the optimal donor for survival, we have now expanded our remit to also include patient-led research that considers quality-of-life outcomes as an additional priority. We also have a new focus on cell and gene therapies to improve understanding of the best donor, cell source and cell type for these new treatments.

This research cannot and must not be done in isolation. For this reason, we will work to enhance collaborations across the world and across different sectors to help deliver practice-changing clinical trials and to ensure our patients benefit from research breakthroughs, wherever they take place. We’re also working to ensure research policy supports the needs of transplant patients.
Finally, we are investing in future talent, without which achieving our goals wouldn’t be possible. We’ve committed to education and training programmes, including postgraduate degrees and fellowships, to help us future-proof international expertise in haematopoietic stem cell research. Through this team, we will continue to embed the highest standards of research culture – such as including patient and donor voices at every stage of the research process.
HLA-matching is the cornerstone of HCT. However, owing to the complexity and diversity of HLA genes, some patients have unique genetic types for which an ideal donor is highly unlikely to be found. Crucially, our research shows that patients from minority ethnic backgrounds are more likely to have rare genetic types, making it harder to find them an HLA-matched unrelated donor compared to those with white or Northern European heritage.10
Organisations across the globe, including Anthony Nolan, are working hard to recruit more people of minority ethnic backgrounds to help address this disparity. As a founding member of the World Marrow Donor Association (WMDA), we are part of a network operating in 55 countries, with access to over 40 million adult donors.11
Yet, studies of HLA and population genetics shows that these staggering numbers alone, even with further recruitment, will not be enough to find everyone their perfect donor.12 To level the playing field, we must find alternative solutions when an HLA-matched donor cannot be found.

Unrelated donor umbilical cord blood has been an important alternative source of haematopoietic stem cells for many years. This blood, which is otherwise discarded after birth, is rich in stem cells and can withstand a lower degree of matching than cells taken from adult donors.13 Since the first successful transplant with cord blood in 2012, over 300 transplants have taken place in the UK.13 However, the specialist clinical knowledge required to administer cord blood donations, combined with factors like lower cell dose, mean that umbilical cord blood is not a suitable alternative for every patient.14,15
Recent advances in transplant practice and new strategies to prevent graft-versus-host disease, such as post-transplant cyclophosphamide (PTCy), are another important option. Use of PTCy now allows patients to receive an allogeneic HCT from an HLA-mismatched donor, either related haploidentical or unrelated, in a way that was not previously possible.16
Ongoing clinical trials, which Anthony Nolan is helping to support, are assessing the safety and efficacy of PTCy in both matched and mismatched unrelated donor transplants.17,18 While further research is needed to understand the long-term consequences of this approach, results so far show that PTCy is significantly increasing donor options for those without an HLA-matched unrelated donor, with very encouraging clinical outcomes.16
Beyond finding a donor, we are also interested in whether other factors – such as socioeconomic status, household income, educational level and regional location – also influence HCT outcomes and survival.
For example, recovery from transplant can be a lengthy process, with many patients requiring long stays in hospital and extended periods of recuperation at home. Those on lower incomes may face more pressure to return to work prematurely, which could impact their recovery. They may also be disproportionately affected by the costs associated with a transplant – some patients have told us that they considered postponing or even refusing a lifesaving transplant due to the financial implications.
Despite this, currently in the UK there is no widely accepted method of routinely collecting information about socioeconomic status and how it may affect quality of life or survival post-transplant.
Our researchers are leading the charge to address this. The Anthony Nolan study SEQoL is pioneering methods for collecting patient-reported outcome data and linking this to socioeconomic factors, aiming to inform how the transplant community can offer the best support possible to every patient.
It’s well accepted that, to fully understand and equitably improve patient experience, those who are affected must be actively involved in research.19
At Anthony Nolan, acting as an advocate for the needs of patients has always been central to our mission. Our unique position as a research institute, facilitator of the world’s oldest register and delivery partner at every stage of the clinical pathway means that we can ensure the diverse views of patients, families and donors are included at every stage of making improvements to care.
We’re also working to ensure diverse patient experiences are factored into research beyond Anthony Nolan – for example, by championing better, more inclusive clinical research practices.
Since the inception of the Anthony Nolan charity 50 years ago, there has been unprecedented progress in outcomes and survival from stem cell transplants. Based on our understanding of his condition, if Anthony Nolan needed a donor today, we estimate he would have as much as a 93% chance of finding a 9/10 or 10/10 HLA-matched donor on our register. But until we see equivalent progress in every patient – regardless of their ethnicity, socioeconomic status and more – there is more work to be done.

References available on our website.
Return to October 2024 Bulletin
Read next
Inequalities in cancer – an unequal burden
17 October 2024
Tackling ethnic inequalities in precision and genomic medicine
17 October 2024