- Published:
- 22 April 2025
- Author:
- Dr Geraldine Boyle and Dr Joseph Houghton
- Read time:
- 4 Mins
In this article, Dr Geraldine Boyle and Dr Joseph Houghton present how changes in assessment can raise the profile of pathology.
In 2023, educators at the Queen’s University Belfast (QUB) School of Medicine posed the question, ‘Is it possible to assess histopathology in an objective structured clinical examination (OSCE) station in undergraduate medicine?’.1 This question arose in response to the implementation of QUB’s new undergraduate medical syllabus (C25), which resulted in a significant reduction in the amount of pathology teaching and written assessment there. The histopathology OSCE was introduced as one strategy to mitigate this loss of visibility.
The impetus behind the C25 curriculum reform was multifaceted but essentially recognised a need for innovation in medical training to better meet 21st century healthcare challenges.2 These challenges were emphasised in national guidance3 that recommended integrated patient care in a context of growing co-morbidity and in local guidance in Northern Ireland,4 which emphasised patient-centred services, ‘blurring’ of primary and secondary care and a focus on population health and prevention.2–4 The new curriculum identified a need for ‘better integration of learning’ between theory and clinical practice and introduced ‘helical themes’, ‘longitudinal clerkships’, increased exposure to primary care, case-based learning and progress testing.2
A more integrated approach means that while pathology is now taught throughout years 1–4, teaching hours have been reduced by more than half. In terms of written examinations, the previous syllabus featured 2 pathology assessments (years 1 and 3) equating to 150 minutes and comprising short questions and multiple-choice questions (MCQs). The new syllabus reduced pathology written examination time to only 28 minutes in total, within a number of integrated exams. Since assessment is a key driver of learning, this reduction is very significant.5,6
The loss of visibility of pathology within an integrated medical syllabus is not a new problem. In 2008, Domizio observed that pathology is often perceived as a fact-based science and, as a consequence of the move from largely ‘didactic discipline-based teaching’ towards ‘integrated systems-based’ teaching, this has led to drastic cuts in pathology teaching.7 McMahon et al. identified that changes to teaching and assessment in the undergraduate curricula over the past 20 years had, by 2008, ‘reduced pathology teaching in most medical schools’ and advised raising the profile of pathology by providing positive role models and through active involvement in assessment.6
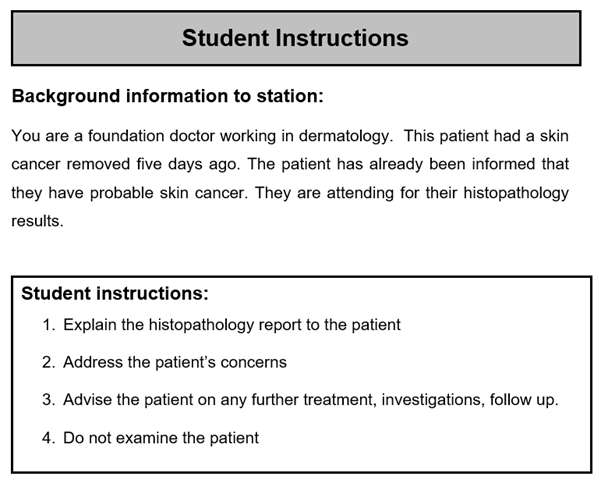
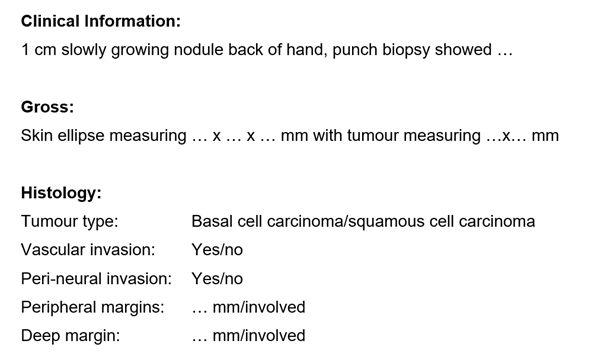
OSCEs and objective structured practical examinations (OSPEs) used to assess clinical competencies can and have been adapted in other undergraduate courses to assess pathology competencies – for example, death certification.5,6 A dedicated histopathology OSCE station (Figures 1 and 2) was trialled at QUB in 2023 as part of third-year undergraduate OSCEs. The station used a skin cancer resection histopathology report as a basis to assess the student’s ability to understand and explain laboratory results, further investigations, treatment and follow-up, while also addressing the simulated patient’s questions and concerns. Psychometric analysis of student marks showed the station was reliable. The OSCE was effective in assessing communication skills, empathy, knowledge of pathophysiology, and aspects of histopathology, e.g. tumour subtype and surgical margins. Following this successful trial, histopathology OSCEs are now used routinely in QUB.
Pathology ‘bridges the gap between basic sciences and clinical medicine’ and provides a framework to understand disease, clinical signs and management.7 The GMC’s Outcomes for Graduates states that ‘newly qualified doctors must be able to apply biomedical scientific principles, methods and knowledge to medical practice and integrate these into patient care’.3 While a minority of students will pursue careers in pathology, many more clinicians will interact with histopathology and reporting, and must have an appreciation of its role and an understanding of its language to facilitate communication and better care, making OSCE an apt form of examination.7 The structure can be easily adapted to assess a range of disease processes and aspects of pathology, including screening programmes.1
As medical undergraduate curricula reform to meet the challenges of healthcare in the 21st century and adopt an increasingly integrative approach, it is important to find ways of maintaining the visibility of specialties like pathology. Additionally, it’s important that training pathways showcase the pathology workforce, particularly through subject exposure and contact with working pathologists as positive role models, to ensure that the next generation of pathologists are enthused about this career.6,7 Histopathology OSCEs are an effective way of assessing knowledge and competency, while also maintaining visibility of pathology.
References available on our website.