- Published:
- 20 January 2025
- Author:
- James Hatcher
- Read time:
- 8 Mins
In this article, James Hatcher of Great Ormond Street Hospital for Children highlights some of the key challenges in paediatric infection practice, focusing on clinical, diagnostic and workforce issues, and exploring examples of how some of these are being addressed.
|
Box 1. Summary of the main challenges in paediatric infection practice. Clinical
Diagnostic
Workforce and recruitment
|
The provision of infection expertise spans a variety of specialties, involving the disciplines of virology, microbiology, infectious diseases, tropical medicine, infection control and public health. Professional bodies across medicine, nursing and healthcare science provide support and training in these disciplines. Among this complex web, there are specialist areas, such as paediatrics, that need specific infection input due to their unique clinical and diagnostic issues.
The British Infection Association, the Royal College of Pathologists and the Royal College of Physicians published best practice standards for the delivery of NHS infection services in the United Kingdom in 2021.1 The aim of the document was to provide standards intended as a benchmark for consistent high-quality infection services. The document noted that most infection diagnostic laboratories will process paediatrics samples, which may have different requirements, so they were outside the scope of the standards.
This article highlights some of the key differences between adult and paediatric practice in infection, clinical, diagnostic and workforce challenges, and offers examples of how these challenges are being met.
Clinical infection management in paediatrics requires specialist knowledge of the differences in clinical presentations, antimicrobial prescribing and therapeutic response compared with adult medicine. Immunodeficiency (primary or secondary) has a profound effect on infection presentation. This is more marked in paediatric practice, which is reflected in the amount of time studying clinical immunology in paediatric infectious diseases training. High-quality evidence on which to base clinical decision-making often lags behind adult practice; there is an unmet need for clinical trials to provide more timely, evidence-informed care in paediatrics.
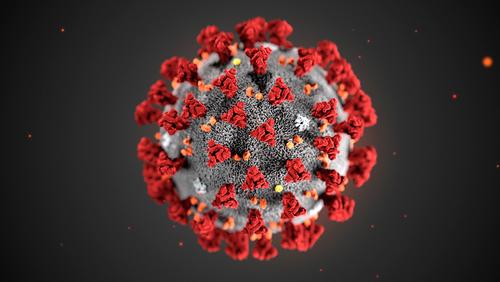
Paediatric evidence for COVID-19 therapeutics
Prior to the COVID-19 pandemic, an estimated 90% of therapies provided for children were yet to be tested in clinical trials; 62% of paediatric trials were delayed or incomplete.2 Post-marketing authorisation of therapeutics in paediatrics was much less likely to be completed. This has led to evidence being borrowed from adult practice to assume the efficacy of treatments in many paediatric infectious conditions.
During the COVID-19 pandemic, there was increased advocacy for more diversity in clinical trials, which led to the US Food and Drug Administration publishing guidance on Bayesian trial design to support this. The guidance aimed to encourage the earlier inclusion of paediatric patients in studies and build a more timely and robust evidence base for future therapeutics.
Antimicrobials
The combination of adult and paediatric patients within a whole-of-life clinical trial is exemplified in the ongoing Staphylococcus aureus Network Adaptive Platform (SNAP) trial, which contains a paediatric cohort (SNAP-PY).3 This international, multicentre, pragmatic, adaptive platform trial addresses multiple questions simultaneously and allows information to be shared across trial age groups. Novel trials such as this may go some way towards reducing age-based exclusion in clinical trials.
Antimicrobial stewardship (AMS) and prescribing principles differ in paediatrics. Consumption metrics, benchmarking, pharmacodynamics/pharmacokinetics, formulations, dosing complexities and limited drug approvals remain significant challenges. In addition, antibiotic exposure in children is associated with long-term effects including obesity and inflammation, alterations in the microbiome and increased risk of superadded viral and bacterial infections. The European Committee on Antimicrobial Susceptibility Testing (EUCAST) released guidance on recommended doses (standard and high) of antibiotics for adults in 2016; however, there are still no consensus recommendations for paediatric dosing.
The acknowledgement of differences in AMS and the paucity of international guidance on antimicrobial choice and doses have led to several specific initiatives within the UK. The UK Paediatric Antimicrobial Stewardship network was set up in 2019 to provide a means of shared learning and to develop guidelines.
In partnership with the British Society for Antimicrobial Chemotherapy, a set of pathways for common paediatric infection management and national antimicrobial prescribing guidelines were developed.4 In 2023, a set of 10 recommendations via multinational consensus was published for AMS in hospital settings for children.5 This will hopefully provide an achievable framework for benchmarking AMS in the future.
An article in the July 2021 Bulletin explored the evolution of paediatric laboratory medicine.6 While paediatric and perinatal pathology is recognised as a separate discipline within histopathology, there is also a need to recognise the distinct differences between adult and paediatric practice across other disciplines, such as clinical biochemistry, haematology, immunology and infection.
There are significant challenges in specimen collection that are unique to paediatrics. Sputum collection is difficult in young children; the use of naso-pharyngeal aspirates can lead to contamination with normal oro-pharyngeal flora. Mid-stream urine samples are the gold standard for diagnosing urinary tract infections but obtaining clean catch urines in young children takes perseverance and is often not possible. Urinary catheter samples are rare in children, usually used in severe illness or complicated urinary tract pathology or post-surgery; therefore, their relative importance is often greater than in adult practice. Blood volumes for all tests are usually small and paediatric laboratories are set up for specialist handling of low-volume samples.
Blood culture volume is critical for pathogen isolation. The misconception that children have higher levels of bacteraemia than adults, and that thus a lower volume is sufficient, leads to lower diagnostic sensitivity. A large study in Kenya showed that, in children aged <13 years, the proportion of positive blood cultures significantly increased with each millilitre of blood (5.6% at 1 ml, 6.8% at 2 ml and 7.9% at 3 ml).7
Paediatric blood culture bottles optimise the blood to broth ratio for low-volume samples and differ in broth formulation to support fastidious organisms. Owing to the low incidence of anaerobic sepsis in children, it remains unclear whether low-volume samples should be split across blood culture bottles or prioritised for more common aerobic organisms.8
The interpretation of common diagnostic tests can be significantly different in paediatrics. Asymptomatic carriage of C. difficile is common in children, especially under the age of 2 years. While clinical symptoms and therapeutic options are similar to adults, the high rates of viral co-infection and asymptomatic carriage of non-toxin- and toxin-producing strains lead to false positive results and over-treatment. Streptococcal urinary antigen tests are recommended in the diagnosis of moderate or severe community-acquired pneumonia in adults but have low specificity in children due to the high rate of colonising Streptococcal species, which reduces the clinical utility of the tests.9
Medical careers in infection have evolved over the past decade to produce more clinically focused physicians. Currently, trainees must complete the foundation programme, a period of internal medicine training and then combined infection training across infectious diseases, medical microbiology/virology and tropical medicine before entering higher specialist training.10
Paediatric trainees previously used to be able to enter pathology by training in microbiology; however, this route is no longer available. Interest in paediatrics will, therefore, need to develop within training. There are limited training options and opportunities for exposure to paediatrics compared to adult medicine. This is compounded by a separate paediatric infectious diseases specialty, which has comparatively little exposure to laboratory-based diagnostics.
Clinical scientist training pathways are led by the National School of Healthcare Science and usually start with the Scientist Training Programme (STP) followed by Higher Specialist Scientist Training (HSST) to become a consultant-level clinical scientist.11
The STP is a 3-year programme of work-based learning, supported by a university-accredited master’s degree. The aim of the STP is to produce graduates possessing the broad knowledge, skills and experience required of a newly qualified clinical scientist. The HSST programme is a bespoke, 5-year training programme supported by a doctorate-level academic award and royal college exams. Exposure to paediatric infection management will often depend on the institution where the trainee is based.
The combination of lack of exposure to paediatrics in both medical and clinical scientist training, no route for paediatricians to enter laboratory-based medicine and lack of exposure to laboratory medicine in paediatric infectious diseases means that future posts in laboratory-based medicine for paediatric infection specialties will be less attractive and may struggle to recruit. This will be especially challenging in standalone paediatric hospitals.
The continued requirement to treat known pathogens in hosts undergoing modern medical interventions, or unknown pathogens such as novel viruses and those with extreme antimicrobial resistance, provides an exciting and evolving field of medicine. Infection expertise needs to adapt to these clinical and diagnostic challenges, while providing a stable workforce.
Clinical trials should include paediatric patients at the outset. Newly established networks must advocate for paediatric AMS at a national level. Future diagnostic methods must be validated for paediatric samples and address low-volume samples, while retaining high levels of accuracy. Finally, professional bodies will need to continue to support this development and work together to address training needs across medical and scientific careers to deliver high-quality infection services into the future.
References available on our website.
Return to January 2025 Bulletin
Read next
Beyond the tooth: The far-reaching impacts of dental caries
20 January 2025



