- Published:
- 20 January 2025
- Author:
- Rosie May-Bennet,Nikul Patel and Heather Lundbeck
- Read time:
- 15 Mins
In this article, Rosie May-Bennett, dental core trainee, along with Heather Lundbeck, clinical lecturer and honorary registrar in paediatric dentistry, and Nikul Patel, clinical lecturer in oral microbiology, underline the importance of a preventative approach to dental caries in children and good antimicrobial stewardship – antibiotic treatment is not normally indicated.
Dental caries remains a major public health issue, being the most prevalent chronic condition among children1 and the leading cause of hospital admissions in 6–10 year olds.2 Moreover, the use of general anaesthesia to manage caries poses significant risks, including potentially life-threatening complications.3
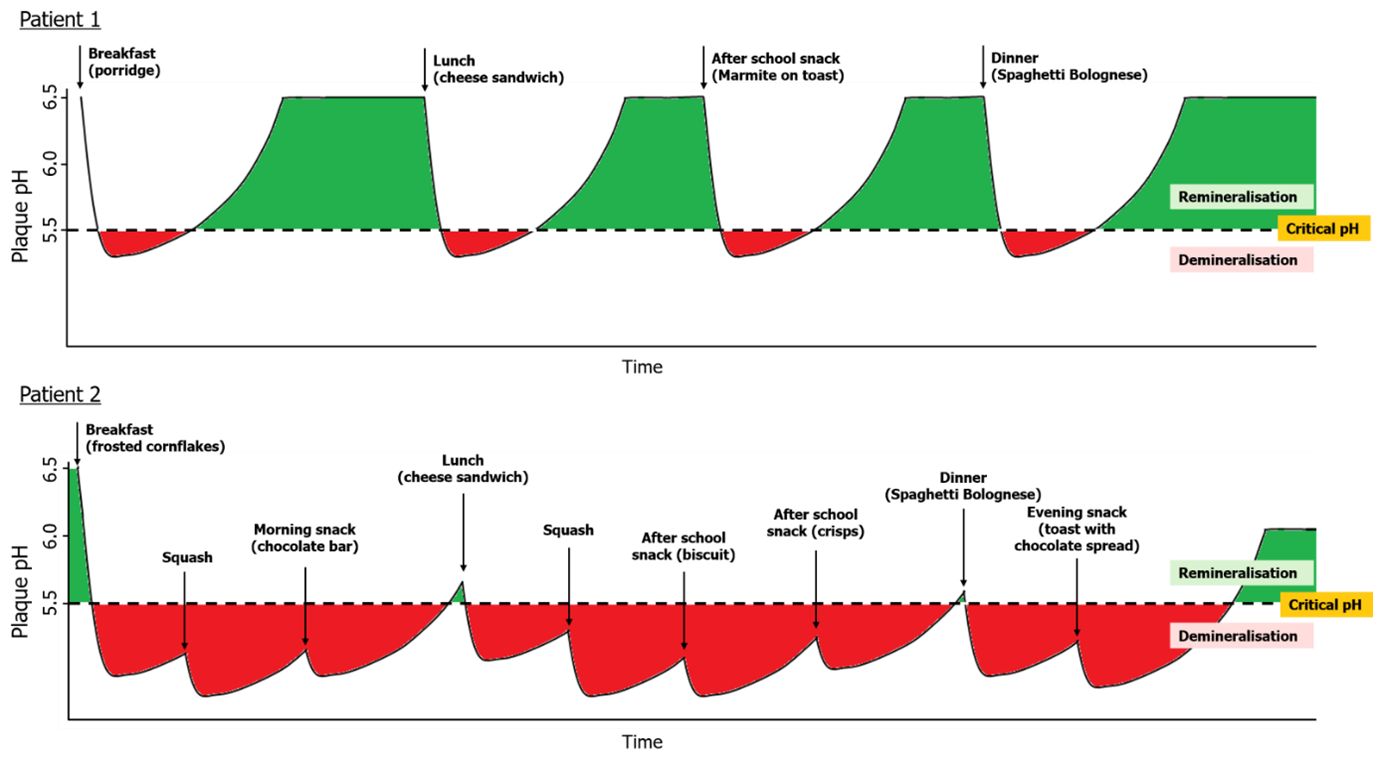
Nearly 50% of 0–6 year olds worldwide have caries,4 accounting for over 500 million children as seen in Figure 1.5 In 2022, nearly 30% of UK 5-year-olds had caries, with rates reaching 40% in deprived areas.6 Despite a reduction since 2008, recent data shows an overall regression over the last 7 years,7,8 likely worsened by pandemic-related declines in dental visits.9 Furthermore, in Wales over 30% of 5-year-olds have caries, while in Scotland 10% of children have severe caries or an abscess.8,10
Figure 1: Estimated prevalence of dental caries of deciduous teeth per country.
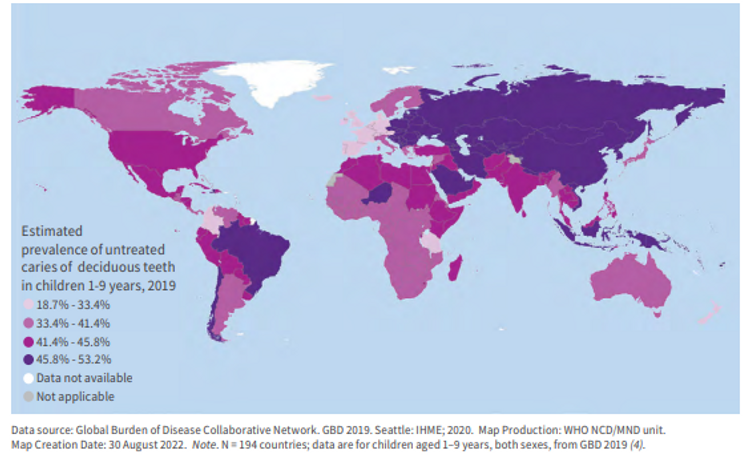
Figure 2: Factors leading to dental caries.
Dental caries, the most common non-communicable disease globally, requires 4 elements to occur: a susceptible tooth surface, plaque, time and substrate (Figure 2). As such, poor oral hygiene, high sugar intake and low pH are substantial risk factors for caries.11
What causes caries?
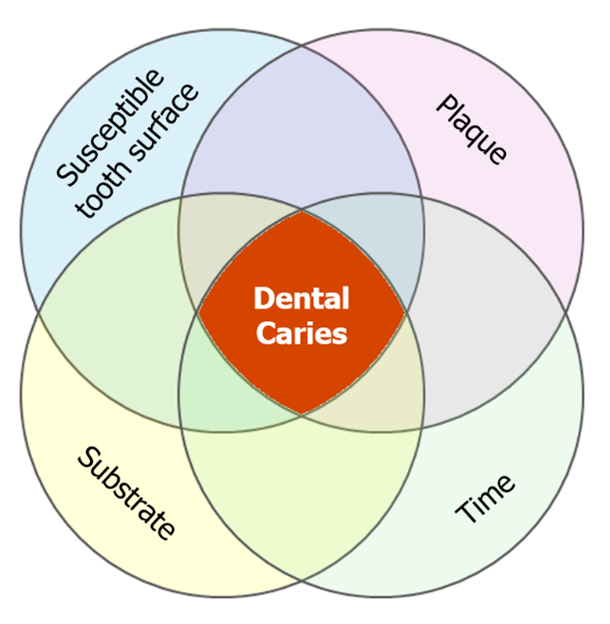
Streptococcus mutans, Streptococcus sobrinus and lactobacilli are the predominant species responsible for caries. The Ecological Plaque Hypothesis explains the shift from health to disease as pathogenic species out-compete symbiotic ones, creating a microbial imbalance within the plaque biofilm. This results in a disease state, in this case, caries. In 1943, Stephan described a phenomenon whereby the plaque biofilm exhibits a rapid and substantial drop in pH following a sugar rinse, caused by acid production from bacterial digestion of fermentable carbohydrates.12,13 Dental enamel has a ‘critical’ pH of 5.5, beyond which it will dissolve. Figure 3 shows the effect of frequent snacking of sugary foods on the pH of the biofilm at the tooth surface.
Patient 1 demonstrates a healthy diet of 3 main meals with a single low-sugar snack. Their plaque pH only fleetingly drops below the critical pH, giving little opportunity for demineralisation. Many hours spent in the green indicates ample time in a higher pH environment, allowing teeth to remineralise.
Patient 2 is high-risk for caries. They are prone to grazing on foods and sipping sugary drinks throughout the day. The high sugar foods lead to a more significant drop in pH and the increased frequency of sugar results in an almost constant acid attack. With minimal opportunity for the pH to return to a safe level, demineralisation outweighs remineralisation, while also providing the pathogenic bacteria with abundant carbohydrate, contributing further to the caries disease process.
Carious lesions can be described as initial, moderate or extensive depending on the depth to which the caries has penetrated (see Figure 4). We now know that earlier lesions can remineralise without the need for any removal of tooth structure, unlike a conventional filling. Fluoride works in 3 ways to achieve this: it inhibits enolase (a bacterial glycolysis enzyme), makes bacteria less tolerant to acids by modifying membrane permeability,14 and becomes incorporated within dental enamel during remineralisation. Under favourable conditions, fluorapatite (a fluoride-enamel hybrid) forms making the surface stronger against caries. The pH at which caries begins to take place changes from 5.5 to 4.5, thus making the tooth more resistant to the disease.15,16
Treatment
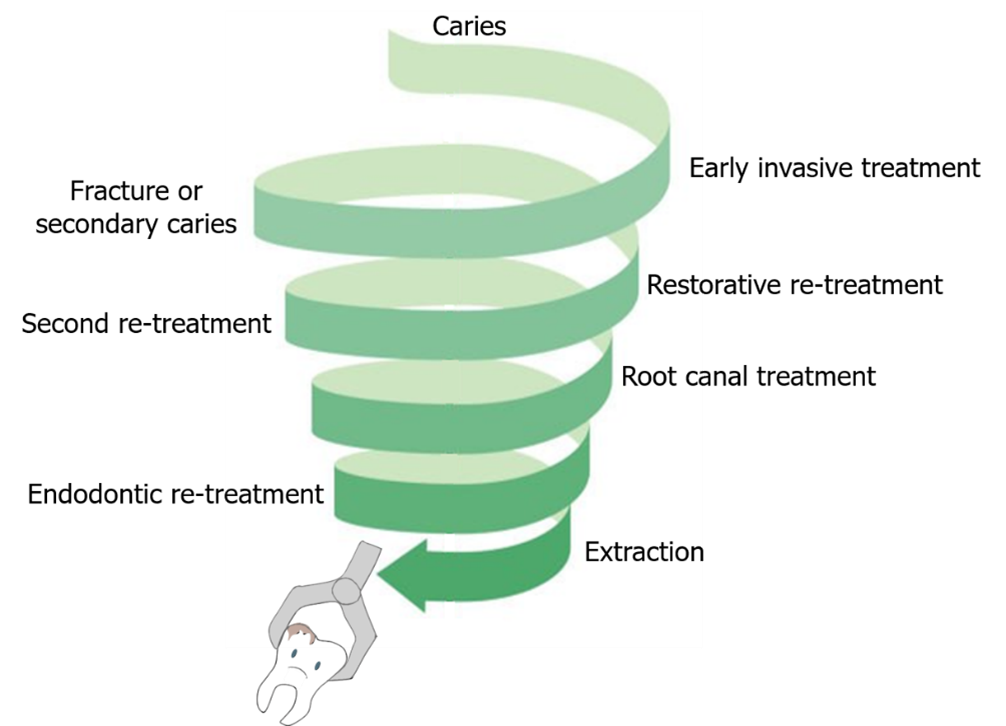
Reversal of caries is important, as most fillings require replacement due to secondary caries or marginal breakdown, where new caries begins between the filling and the tooth. With each replacement, the filling becomes larger. This leads to more invasive procedures such as root canal treatment, which isn’t always successful, and eventually tooth loss. A visual representation of this is demonstrated in Figure 5.17,18
Dental treatment also costs money. Those most affected by caries, commonly from a lower socio-economic background, often cannot afford dental treatment and are more likely to opt to remove the tooth when free or affordable care is not available.
In children, the impacts of early tooth loss include crowding or impaction of permanent teeth, leading to orthodontic treatment. It can also cause low self-esteem due to poor aesthetics.
Figure 4: Stages of caries as per the International Caries Classification and Management System.
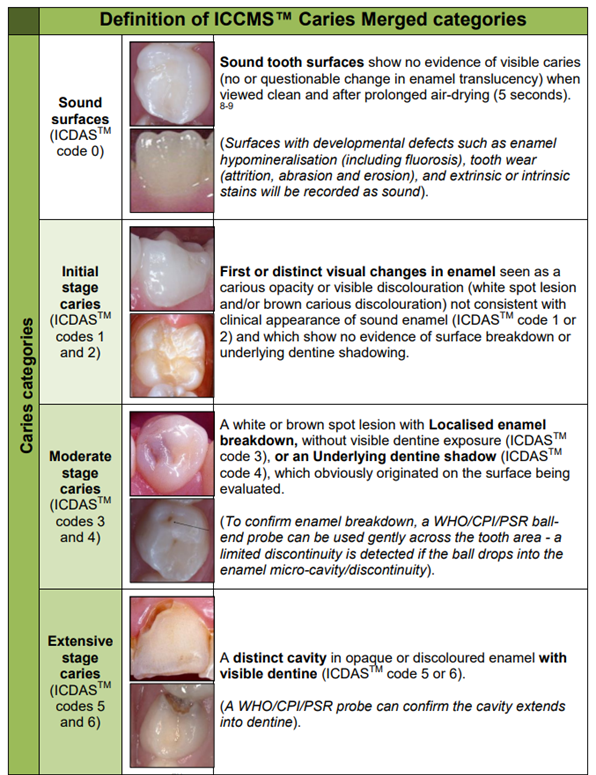
Figure 5: The restorative cycle.
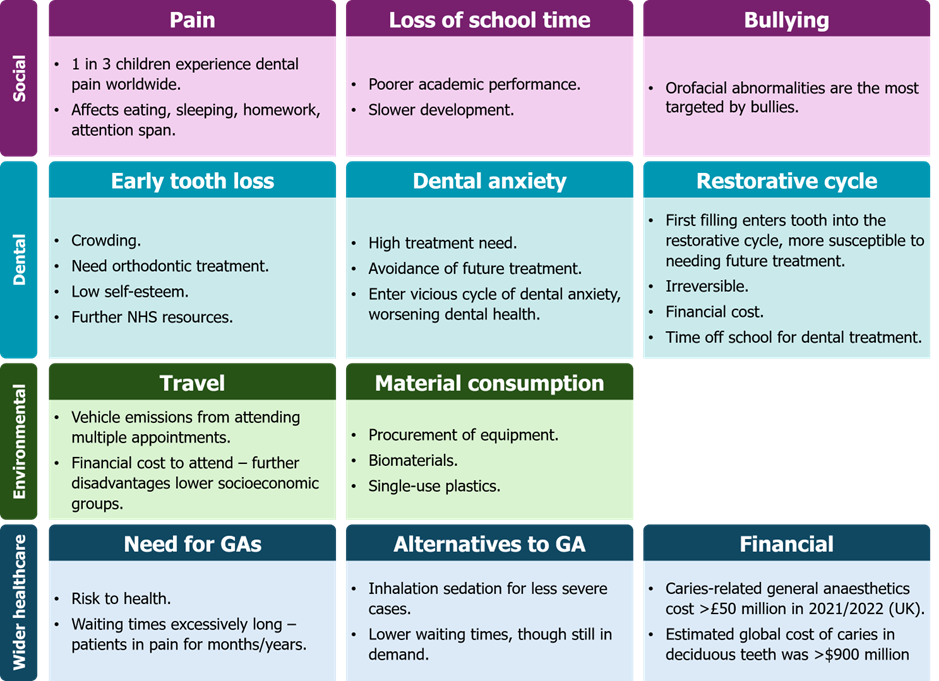
Knock-on effects of caries are vast; health issues are a drop in the ocean. From psychosocial consequences to environmental impacts to financial loss, there is an abundance of negative outcomes.
In the academic year 2022/2023, over 1 in 10 Year 6 students reported dental pain and nearly 20% of parents felt it affected their child’s quality of life.8,20 Paediatric patients in pain are often pre-cooperative (anxious and fidgety), making chairside dental treatment impossible. Therefore, parents often seek antibiotics believing these will help their child’s pain. These are not indicated and will not be effective unless a systemic infection is present. Dentists are responsible for over 10% of antibiotic prescriptions.21 With antibiotic resistance on the rise, antimicrobial stewardship and appropriate prescribing is crucial.
Children requiring procedures under general anaesthetic are added to waiting lists but remain in pain unless they cooperate for treatment, until the tooth dies. Even then, there is potential to flare up again and cause further discomfort. This can affect their eating and drinking, possibly increasing the risk of developing nutritional deficiencies due to selective eating. This may be the beginning of a cycle of further worsening oral health; malnutrition is positively associated with worse oral health outcomes.23 Wider effects of chronic dental pain are highlighted in Figure 6.
Figure 6: Wider effects of childhood caries.
Prevention efforts in healthcare are often classed as upstream, mid-stream or downstream. See Figure 7 for some examples of current UK schemes.
Figure 7: Examples of Public Health initiatives and dental chairside interventions to reduce and manage caries.
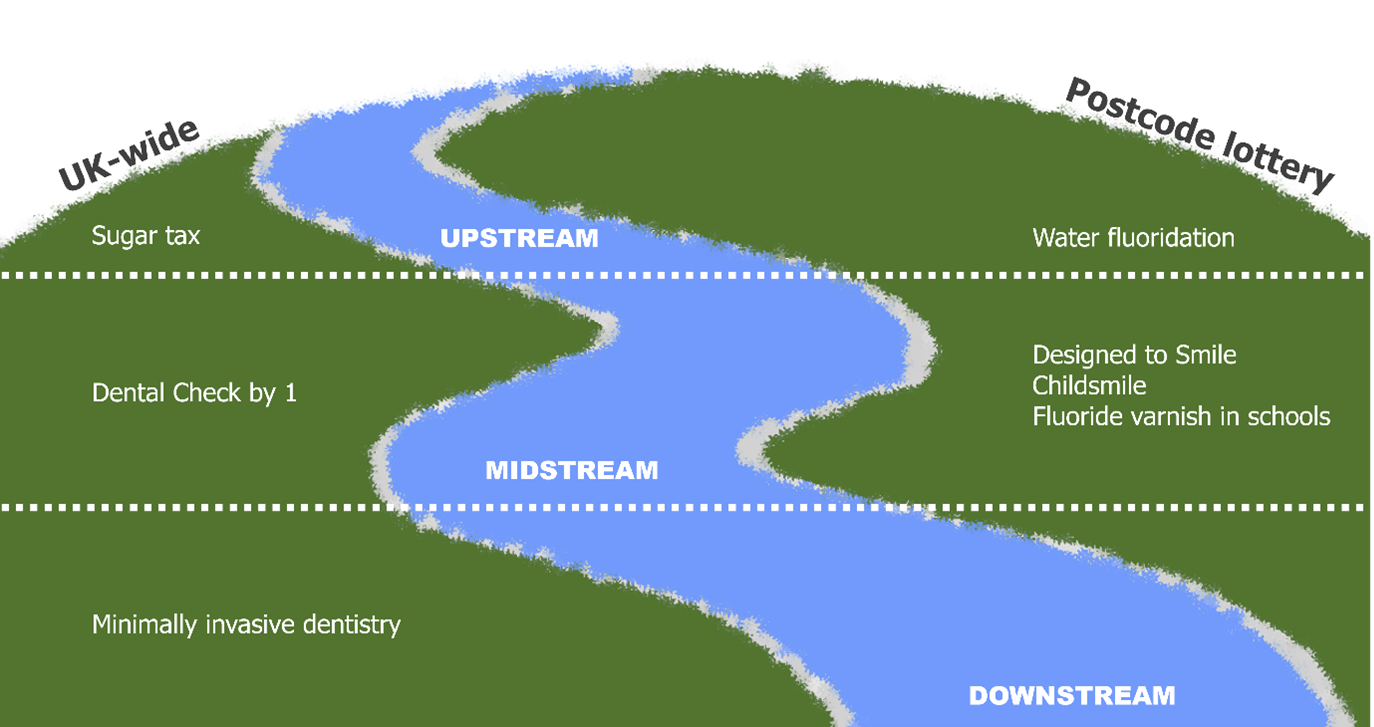
Sugar tax
The UK Government introduced a Soft Drinks Industry Levy in April 2018, increasing tax on companies producing high-sugar drinks. This forms part of a larger campaign to combat obesity by discouraging such drinks and using the tax revenue to fund physical activity in schools.30 Anecdotally, the sugar tax delivered dental health benefits too, though sadly no funding has been translated to dental care, which is often overlooked for healthcare funding.
A review of the levy was recently announced, proposing changes including lowering the existing high sugar threshold and creating a new tax band for drinks containing >10g sugar/100ml. It is unclear where this additional revenue will be allocated.33
Water fluoridation
Despite its proven benefits in preventing caries, especially in children, water fluoridation has a tumultuous history.34 The World Health Organization stipulates fluoride levels in drinking water should not exceed 1.5 mg/L; water fluoridation schemes usually aim for 1 mg/L.35 In England, only 10% of the water supply is fluoridated to at least 0.7 mg/L, while Scotland, Wales and Northern Ireland have no water fluoridation schemes.36 Public Health England hypothesised that if fluoride concentrations increased from 0.2 mg/L to 0.7 mg/L, caries could be reduced by up to 28% in the most deprived groups.34,37
Arguments against water fluoridation include increased fluoride during tooth development can causing dental fluorosis, where teeth become mottled or discoloured. However, this is unlikely at the proposed low dose.38 Other anecdotal associations include neurological harm and hypertension, though this evidence is low-quality.39
Public health programmes
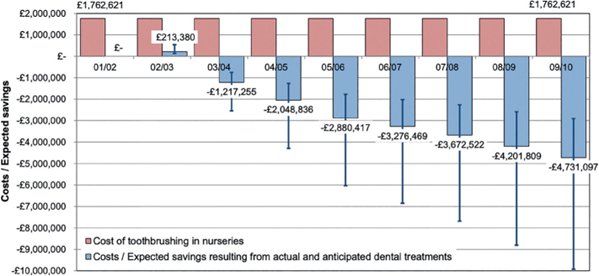
Designed to Smile and Childsmile are public health programmes which deliver toothbrushing support in schools across Wales and Scotland respectively. During the last academic year, Designed to Smile distributed over 160,000 toothbrushing packs, with nearly 60,000 children participating in toothbrushing programmes in primary school or nursery.31 In Scotland, 50% of primary schools and 86% of nurseries participated in Childsmile’s toothbrushing programme in 2022/2023.32 Due to their preventative success, these initiatives should be seen as cost-saving investments (Figure 8). For example, nursery toothbrushing schemes in Scotland cost Childsmile £1.8 million per year, though after 8 years of investment, the savings are estimated to be over 2.5 times this amount every year.40
Figure 8: Costs versus expected savings of Childsmile.
It is crucial that families receive support early, as prevention is preferred to treatment. The British Society of Paediatric Dentistry endorses ‘Dental Check by One’ (DCby1), encouraging children to be seen by a dentist by the age of 1.29 DCby1 equips dentists with strategies to better manage ‘pre-cooperative’ children, e.g. allowing the patient to sit on their parent’s lap for examination.41
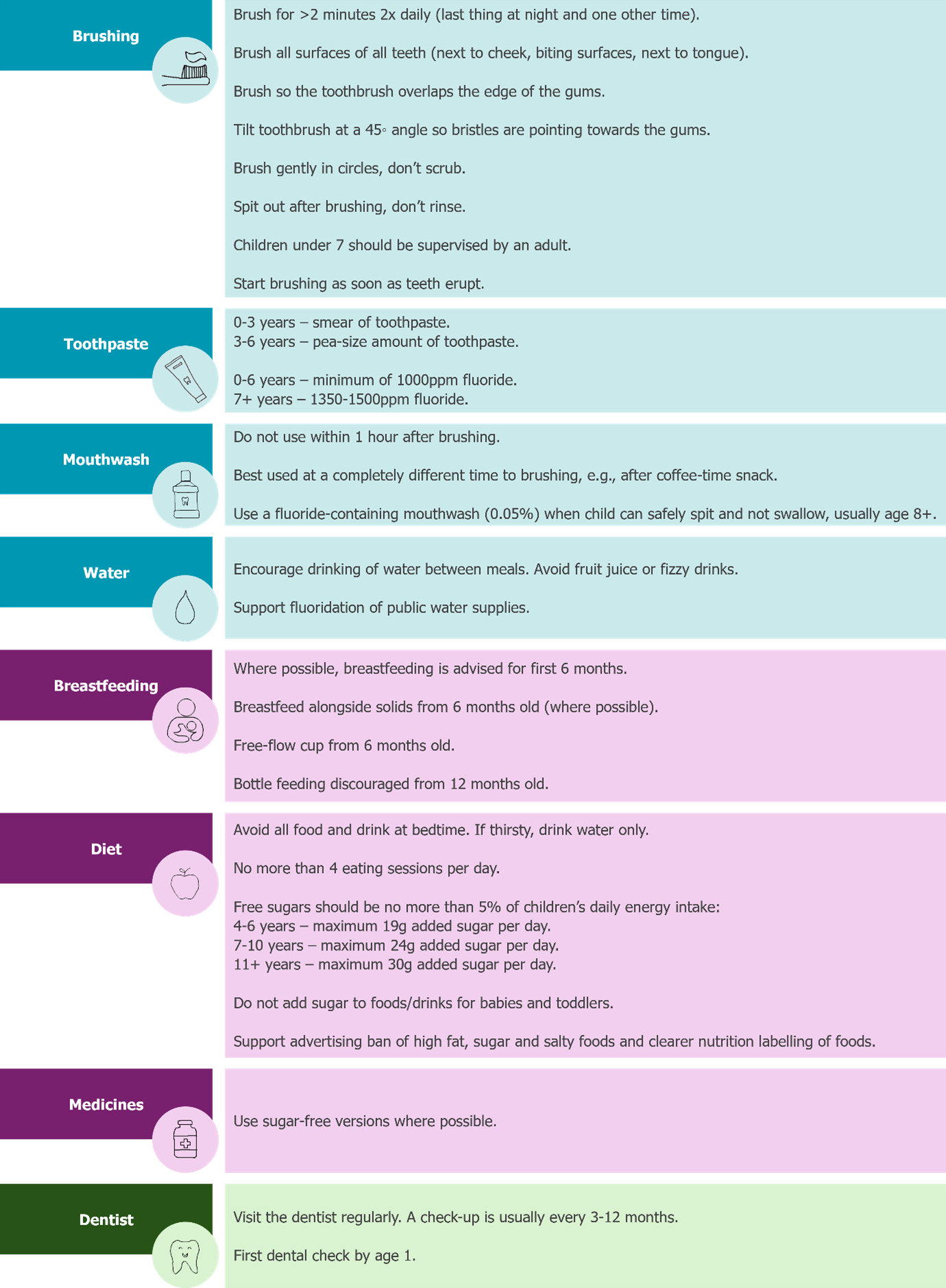
It’s safe to say that no matter the area of healthcare, prevention is better than cure. Caries is largely preventable with excellent oral hygiene and frequent fluoride exposure. People at high risk of caries also share risk factors for other diseases, such as diabetes, therefore it is vital that all healthcare professionals ‘make every contact count’ by delivering key preventative messages, as given in Figure 9.42
Figure 9: Basic caries prevention aids.
It is no secret that accessing an NHS dentist is challenging at present. Patients may seek antibiotics from GPs for dental pain and it must be reiterated that these cannot cure toothache. Medical practitioners should advise for patients to contact NHS 111 for emergency treatment, e.g. severe dental pain or facial swelling, if they are not registered with a general dental practitioner.46–49
By emphasising the importance of the aforementioned habits, we should all be able to make a positive impact on children’s dental health.
References available on our website.
Return to January 2025 Bulletin