Workload and COVID-19
The diverse disciplines within pathology have always been central to the diagnosis and treatment of patients with cancer. However, a Cancer Research UK report from October 20201 estimated that the histopathology workforce needs to increase by 45% by 2029 to meet the needs of the projected increase in cancer workload and case complexity.
The existing workload pressures and the need to adapt conventional workflows to precision medicine approaches have been exacerbated by the efforts now required to address the backlog of work as a consequence of the COVID-19 pandemic. In this issue of the Bulletin, Professor Antonio Pagliuca (pp 469–472) reflects on the challenges the Anthony Nolan charity faced during the pandemic and its continued impact on research and clinical care in complex diseases.
Clinical trials and the SPIRIT-Path project
The 2013 SPIRIT (Standard Protocol Items: Recommendations for Interventional Trials) statement provides evidence-based recommendations for the minimum content of clinical trial protocols and is widely endorsed as an international standard for use by protocol authors.2 Specific protocol elements not fully covered by the SPIRIT statement have been addressed by extensions to the statement, for example, covering the use of artificial intelligence in trials. Pathological confirmation of diagnosis is often required for trial eligibility, particularly in trials of cancer therapeutics, and is still assumed to be the gold standard despite the inherent subjectivity in practice that has neither been codified nor formalised.
In May 2019, the Cellular and Molecular Pathology Initiative (CMPath), under the auspices of the National Cancer Research Institute, commenced the SPIRIT-Path project to develop international consensus guidance for pathology in clinical trial protocols. Although not specific to trials of cancer therapies, the SPIRIT-Path extension will be applicable to a large proportion of trials in oncology, given the reliance on histological diagnosis for trial inclusion or other histopathological or molecular pathology assessments.
Pathological confirmation of diagnosis is often required for trial eligibility, particularly in trials of cancer therapeutics, and is still assumed to be the gold standard despite the inherent subjectivity in practice that has neither been codified nor formalised.
The project has made good progress, despite the global pandemic, and was facilitated by an increasing acceptance of remote working and teleconferencing. In fact, the entire process to completion of the guidelines could probably be badged as ‘carbon neutral’.
The final consensus guidelines have been recently published and their adoption by protocol authors will increase the completeness and quality of trial protocols.3 Interestingly, Dallmann and Varma (pp 461–464) propose a more pragmatic, evidence-based and clinically informative approach to prostate biopsy reporting that may serve to address problems of data completeness and reproducibility if applied to trials.
The CMPath team is now embarking on a follow-on project to develop CONSORT-Path guidelines for the reporting of pathology-related activities to complement the SPIRIT-Path extension. Further, we are developing a Good Clinical Practice training module in ‘Trials Pathology’ with the intention that completion of the training by interested members of staff, irrespective of the nature or location of their department, will build a community of research-ready clinical trial laboratory scientists and pathologists.
Next-generation pathology for precision medicine
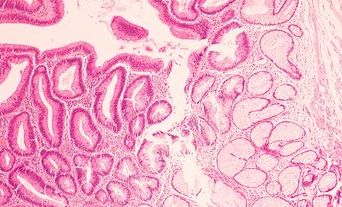
Next-generation pathology will be enabled by technical advances including digitisation, the application of computer vision technology and artificial intelligence, and integration with somatic mutations measured in micro-dissected, quality-assured tissue.
... there is an associated need to develop the next generation of clinical data analysts with the requisite skills to bridge the knowledge gap in this exciting era of ‘big data’ and integrated clinical diagnostics to maximise the clinical value of this new information.
Sosinsky and Walker from Genomics England provide an essential overview of whole genome sequencing (pp 480–482), while Elliot and Jones thoughtfully discuss how this and other next-generation methodologies may be integrated into everyday histopathological practice for greatest clinical benefit, despite the inherent challenges in doing so (pp 483–485). As Davies and Ferry highlight in their article in this issue (pp 466–469), there is an associated need to develop the next generation of clinical data analysts with the requisite skills to bridge the knowledge gap in this exciting era of ‘big data’ and integrated clinical diagnostics to maximise the clinical value of this new information.
This issue also includes examples of best practice with regard to the integration of molecular diagnostics into routine clinical practice, with articles describing the evolution and adoption of molecular diagnostics in lymphoreticular disease and cervical cancer screening (pp 476–479 and pp 464–466). The articles highlight the protracted timelines, conflicts with regulatory frameworks and difficulties implementing such changes into NHS healthcare delivery. Understanding of the specific aberrant pathways underlying the disease of individual patients – particularly with cancer – increasingly informs precision treatments, including advanced cell therapies. Wolf and Griffin’s article (pp 472–475) provides an excellent summary of the use of CAR-T therapies in haematological malignancy.
About the National Cancer Research Institute
The National Cancer Research Institute (NCRI) is a UK-wide partnership of cancer research funders, established in 2001. NCRI works to coordinate research related to cancer, to improve the quality and relevance of research and to accelerate the translation of research into clinical practice for the benefit of patients.
The NCRI Cellular Molecular Pathology Initia-tive (CMPath) was launched in 2016 to reinvigorate UK academic pathology. The initiative was created in recognition of the importance of pathology in drug development and clinical research and aims to change the way pathologists engage with, conduct and are recognised for their work in clinical trials.
For more information visit www.ncri.org.uk.