The Healthcare Safety Investigation Branch (HSIB) conducts independent investigations of patient safety concerns in NHS-funded care across England. Our investigations identify the contributory factors that have led to harm or the potential for harm to patients. The safety recommendations we make aim to improve healthcare systems and processes to reduce risk and improve safety. We work closely with patients, families and healthcare staff affected by patient safety incidents, and we never attribute blame or liability. We undertake patient safety investigations through the following two programmes.
National investigations
Concerns about patient safety in any area of NHS funded healthcare in England can be referred to us by any person, group or organisation. We review these concerns against our investigation criteria to decide whether to conduct a national investigation. National investigation reports are published on our website and include safety recommendations for specific organisations.
Maternity investigations
We investigate incidents in NHS maternity services, including:
- babies born at term, after a woman has gone in labour with a live baby, who experience intrapartum stillbirth, early neonatal death or potential brain damage diagnosed in the first seven days of life
- our HSIB-defined criteria for maternal deaths. Our investigation reports are shared with the family and trust, and the trust is responsible for carrying out any safety recommendations made in the report.
In addition, we identify and examine recurring themes that arise from trust-level investigations to make safety recommendations to local and national organisations for system level improvements in maternity services. For full information on our national and maternity investigations, please visit our website.
In this article, we describe two areas of our work – maternal death and placental pathology.
Maternal death: learning from maternal death investigations during the first wave of the COVID-19 pandemic
In March 2021, HSIB published a national learning report that reviewed findings from investigations
into maternal deaths that met our criteria and occurred between 1 March 2020 and 31 May 2020.1
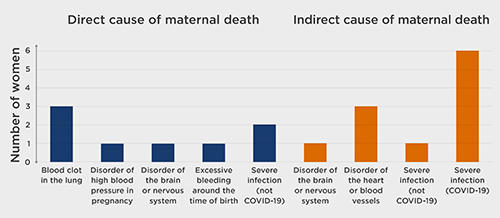
19 families gave their consent for their investigations to be included in the review. The causes of the women’s death are shown in Figure 1.
Families are central to HSIB investigations. The families affected by the deaths of these 19 women identified four areas of concern.
Experience of maternal collapse at home
Circumstances where family members were asked to assist healthcare professionals at home – including assistance with resuscitation of their relative and with use of equipment – had a significant impact. Although there was a clear time-critical imperative for this, and it does occur outside the pandemic, HSIB investigations noted the impact such involvement had on family members.
Visiting restrictions
Changing policies that meant women were alone when attending hospital appointments, emergency departments, assessment units, ultrasound scans and on admission to hospital, including in maternity settings and intensive care units.
Families’ ability to advocate or support
There were instances when families did not have the opportunity to visit the woman prior to her death. Visiting restrictions coupled with the sudden and, at times, unanticipated deterioration of the women’s clinical condition added to the families’ distress.
Families want to understand more about why their relative died
There were situations where families wanted to understand more about why their relative died and felt that information from a post-mortem examination (PME) would have helped. Nine of the women did not receive a PME, with the coroner deciding on cause of death based on other factors such as computed tomography scans or symptoms.
Themes of investigation
Seven themes emerged from HSIB’s analysis of the investigations.
Unprecedented demand for telephone advice caused delays in accessing health care Several women, or their family members, attempted to contact NHS services by telephone. These included NHS 111, GPs and maternity helplines. Families described experiencing significant delays, making repeated attempts and abandoning calls after waiting to connect with an operator.
Public messaging and ‘safety netting’ advice caused delays in seeking healthcare
The message from the UK government during March to May 2020 was to ‘Stay Home. Protect the NHS. Save Lives’.2 HSIB investigations found that women and their families were concerned about their health, the risk of exposing their unborn baby to COVID-19 and the requirement to attend hospital without the support of their families. Because of these concerns they put off going to hospital for longer than they otherwise may have done.
Guidance changed rapidly
The effort to produce guidance to inform clinicians and the public about COVID-19 was unprecedented and the resultant wave of information being directed at staff on the frontline was considerable. It is evident from HSIB investigations that it was difficult for hospital trusts to keep staff apprised of updates to guidance.
Use of early warning scores did not always detect deterioration
HSIB investigations identified that early warning systems were not always used as intended. The issue of compliance in monitoring and recording clinical observations requires an understanding of working practices, and there are complexities in how scoring systems are embedded in practice. There is no nationally agreed maternity-specific early warning score in England, and investigations found examples where the National Early Warning Score (NEWS) 2 score, not designed for use in pregnant women, was used.
Personal protective equipment requirements changed due to COVID-19
The design of work processes and the environment did not adapt to account for the increase in time used to don personal protective equipment (PPE). Environments were described as ‘noisy’ with staff having to repeat requests and seek clarity of instructions. Clinicians’ voices were ‘muffled’, and staff reported ‘heightened stress levels’ because of communication difficulties associated with wearing PPE.
Staff described feelings of stress and distress, which can affect performance
Stress was aggravated, for example by communication difficulties caused by PPE, redeployment to unfamiliar work areas and reduced staffing levels. The report highlights areas where organisational resilience may be increased.
Difficulties in making a diagnosis and choosing treatment strategies
Several investigations highlighted diagnostic challenges that may have resulted in missed or delayed diagnosis. Diagnosis was impeded by lack of communication and face-to-face assessment, access to tests and concerns about infection prevention and control, as well as complexity caused by rapidly acquired knowledge of a new disease and the physiology of pregnancy.
The report concluded that HSIB investigations identified: patient safety risks arising from the disease itself or from behaviour changes relating to patient and staff appreciation of risk, changes in patient pathways and access to services, obstacles to care caused by additional safety precautions such as PPE, and reduced availability of staff.
Safety recommendations
HSIB made safety observations about:
- the need to understand the increased risk of maternal death for women from black, Asian and minority ethnic backgrounds and those with higher socioeconomic deprivation
- the use of the NHS England and NHS Improvement communications toolkit to improve communication with women from black, Asian and minority ethnic backgrounds in all healthcare services for pregnant women
- the development of written safety netting advice for pregnant and post-partum women about COVID-19 and other common conditions, incorporating the MBRRACE-UK (Mothers and Babies: Reducing Risk through Audits and Confidential Enquiries across the UK) recommendations.
HSIB also reiterated a previous safety recommendation made in a report on COVID-19 transmission in hospitals: ‘It is recommended that the Department of Health and Social Care, working with NHS England and NHS Improvement, Public Health England, and other partners as appropriate, develops a transparent process to co-ordinate the development, dissemination and implementation of national guidance across the healthcare system to minimise the risk of nosocomial transmission of COVID-19.’3
The report concluded that HSIB investigations identified: patient safety risks arising from the disease itself or from behaviour changes relating to patient and staff appreciation of risk, changes in patient pathways and access to services, obstacles to care caused by additional safety precautions such as PPE, and reduced availability of staff. HSIB considers effective interventions are most likely to be successful at the system level.
HSIB has initiated national investigations in two areas identified from the review, namely the capacity of NHS 111 to respond to an unprecedented increase in demand and the detection of venous thromboembolic disease in pregnancy.
Placental pathology
Placental histopathology assessment is an important element of care for the babies that meet our referral criteria. HSIB recognises that around 40% of adverse events in babies are associated with placental vascular disorders;4 placental histopathology may reduce the classification of ‘unexplained’ stillbirth from 30% down to 10%5 and placental fetal vascular malperfusion is associated with the risk of neonatal encephalopathy.6
Placental pathology is important in helping HSIB investigations give families an explanation for the outcomes of their babies. It also assists in planning care in future pregnancies, as there may be a chance of recurrence.
HSIB has found that in around half of our investigations, the placenta was not sent for histopathological assessment. In more recent investigations, we observe that more placentas are being sent for examination, which HSIB believes reflects that trusts act on our findings and recommendations.
Families value HSIB maternity investigations for their independence and explanation of events in simple language. One family gave the following feedback: ‘We felt the process has helped us to better understand what happened and the report is written in a way that can be understood by someone who has no medical background’.
The RCPath recommends that placentas that are sent for full examination should include those ‘from stillbirths, fetal growth restriction and cases of severe fetal distress requiring admission to a neonatal intensive care unit’.7 HSIB acknowledges that, in some areas of England, placental pathology services are limited by a shortage of specialist placental pathologists, which influences the ability of a trust to meet this national recommendation.
HSIB has found that in around half of our investigations, the placenta was not sent for histopathological assessment. In more recent investigations, we observe that more placentas are being sent for examination, which HSIB believes reflects that trusts act on our findings and recommendations. A HSIB maternity investigation noted: ‘in combination with the other features seen in this placenta, it is likely that the delayed villous maturation caused longstanding lack of oxygen (chronic hypoxia) in the baby.’
Conclusion
HSIB is working across all healthcare settings to improve patient safety through effective and independent investigations that do not apportion blame.
Recent publications have included a thematic review of maternal deaths during the first wave of the COVID-19 pandemic; the themes identified are relevant to all areas of healthcare. Detailed analysis of maternal deaths is a relatively unique area of investigation − there are few other cohorts of individual deaths that undergo similar assessment.
HSIB’s investigations have highlighted to trusts the importance of placental histopathology and are likely to be influencing improved uptake. HSIB is working jointly with the RCPath and NHS England to understand and overcome the barriers to wider implementation of the RCPath’s Tissue pathway for histopathological examination of the placenta .7





