From dental practice into oral and maxillofacial histopathology
It was a summer family gathering (socially distant of course) where one of my uncles asked me how being a dentist was going in these uncertain times. I didn’t fully appreciate how hard it was to explain pathology as a career – ‘slides not teeth’, ‘samples not patients’; I don’t think I did the best job explaining this or answering why I was no longer a traditional dentist. With some more thought and several cups of tea, let me have another go at explaining it.
The sound of the drill at the dentist or that notable waiting room smell of disinfectant is enough to trigger fear in many patients however for me, it was something I always found fascinating.
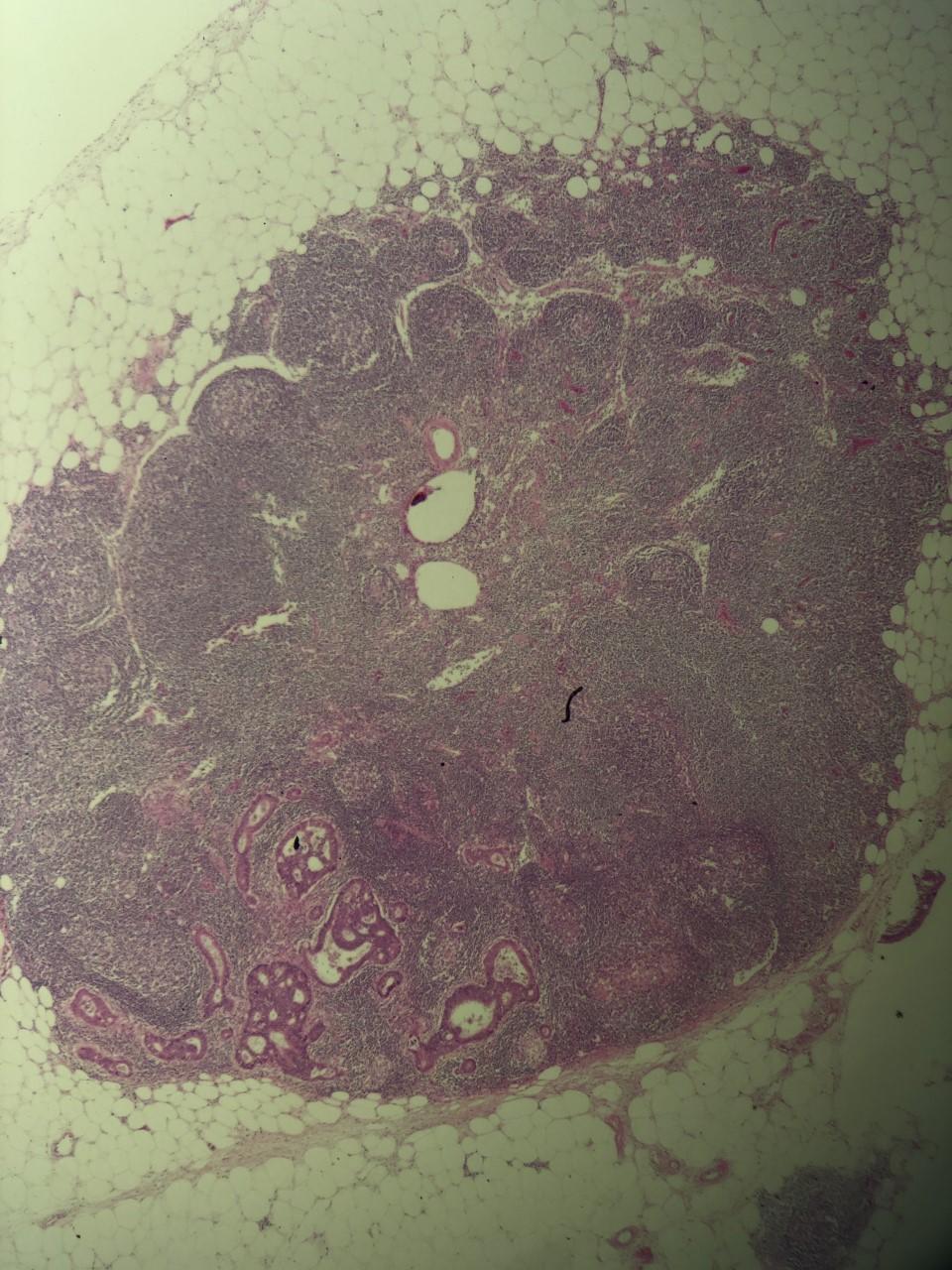
Metastatic Adenocarcinoma (bottom left) in a lymph node.
The sound of the drill at the dentist or that notable waiting room smell of disinfectant is enough to trigger fear in many patients however for me, it was something I always found fascinating. As poetically said by a restorative tutor, dentistry is the perfect marriage between science and surgery. From my own experiences as a longstanding orthodontic patient, I had come to enjoy the profession by looking from the outside-in. After some inspiring work experience and words of encouragement from my own dentist, I took the leap of faith and applied for dental school. Fast forward some A-levels and multiple university interviews; I had accepted the offer to study Dentistry at The University of Manchester.
Time for a career change
I still remember the poignant moment I was getting ready to leave for university, an 18-year-old nervous but excited to start a new chapter in my life. It was the day before I was set to leave with my parents, we were sat in the living room and my parents were sharing their own university stories with me. It was at this moment that my mum noticed a ‘lump’ behind her jaw as she was moving her hair behind her ear. Thinking it was a swollen lymph node with no other symptoms, we dismissed this as nothing of concern.
The new dust from moving into university halls had barely begun to settle and fresher’s week was nearing an end when I received the phone call that the ‘lump’ was too big to be a lymph node and wasn’t going away. I attended the hospital consultation with my mum. We were seeing an Oral and Maxillofacial Surgery Consultant who told us it was a ‘tumour in the parotid salivary gland’. I’m not really sure what was discussed after this, I remember the distinct ringing in my ear and the butterflies that started fluttering in my stomach. Then, that silent drive back, not understanding what was going to happen next.
This was the first time I had even heard of a pathologist but realise the gravity of their report on my families’ future. Ultimately, this event was the spark that encouraged me to undertake an intercalated degree in pathology.
After arriving back in Manchester, I decided that my family needed me more and I was ready to drop out of my University degree. Two senior university tutors had a series of long meetings with me where they helped me understand what was happening from a medical perspective but also provided the reassurance that I would be supported with time away from my studies. ‘We are a family here in Manchester after all’.
After a long operation filled with complications, we were waiting on a pathology report to confirm the diagnosis. This was the first time I had even heard of a pathologist but realise the gravity of their report on my families’ future. Ultimately, this event was the spark that encouraged me to undertake an intercalated degree in pathology.
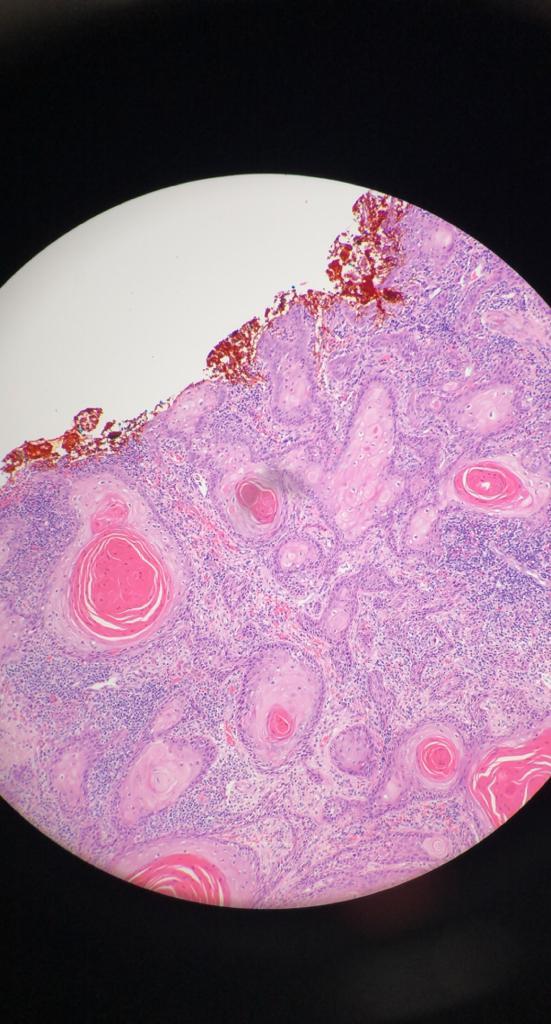
Representative H&E photomicrograph showing an invasive squamous cell carcinoma.
Moving into a laboratory
Leaving my slowly developing comfort zone of dentistry, I entered a laboratory where potions and chemicals were stacked high on bench worktops and white lab coat scientists filled the room. In the microscopic reporting room, tissues from every aspect of a patient’s body were reviewed and examined to determine a diagnosis. Our first exercise was to evaluate an axillary lymph node biopsy that had been taken from a lady. A myriad of colours exploded from the circular microscope field as we slowly turned the wheel to move around and tried to work out what we were looking at (albeit with one eye closed).
You will often read in books, pathology is the ‘gold standard’ but what happens in the room of potions behind the scenes is far more exciting than can be summarised in text.
The consultant explained all the normal features and highlighted the metastatic carcinoma present which was responsible for the swelling. The markers found on a cell surface or specific proteins in a nucleus can be detected using special stains (known as immunohistochemistry) and can help determine where this carcinoma had originated from but to my surprise, some organ cancers have a particular look about them which the experienced eye can detect. ‘This is breast cancer, I can tell by the way the cells look, I just need to confirm this with my stains’ the consultant informed. Sadly for this patient, a lump in her armpit will be the start of her cancer pathway.
The role of pathology: what goes on behind the scenes
Such events are commonplace in a pathology department, samples marked on the 2-week urgent pathway being found benign and the converse, routine excisions that appeared inflammatory showing clear malignancy. The role of the pathologist is more of a detective and does not stop at the diagnosis; grade, stage, features that inform patient treatment (such as lymphovascular or perineural invasion), capsular rupture, hybrid carcinoma’s and transforming tumours all need to be accurately detected and reported. Large surgical resections need to be sampled which requires understanding of anatomy and the surgical procedure, ‘we can’t process everything – there’ll be thousands of slides’ one consultant told me. This was one of my first lessons as a trainee –don’t put it all in the machine! All of this information is digested and conveyed to the surgical and oncology team during multi-disciplinary team meetings.

You will often read in books, pathology is the ‘gold standard’ but what happens in the room of potions behind the scenes is far more exciting than can be summarised in text. Every day, I learn new entities, how they clinically present and what they look like under a microscope, creating a large cerebral filing system composed of thousands of photographs. In my second year of training, I came across a parotid tumour from a patient whose age and circumstances resonated with me. At that moment I realised, it’s now my turn to be the detective.

